“As we understand more and more about the genetic basis and other aspects of the pathogenesis of lymphomas, we will be able to establish more precise and less toxic, more biologically oriented drugs that might have fewer side effects compared to standard chemotherapy.”
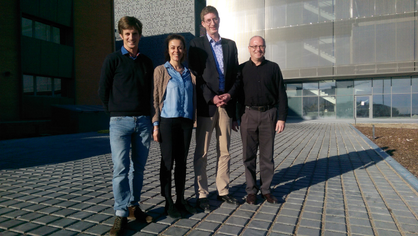
We had the great pleasure of receiving Dr. Andreas Rosenwaldat the Josep Carreras Leukaemia Research Institute’s Germans Trias i Pujol Campus.
Dr Rosenwald gave a talk at our centre entitled ‘The broad molecular and clinical spectrum of follicular lymphomas’
Dr Rosenwald is a hematopathologist and is the head of the Institute of Pathology at the University of Würzburg since September 2009. After starting his scientific career at the Pathological Institute in Würzburg, he researched for four years at the National Cancer Institute in Bethesda, USA.
His main area of research is focused on Hematopathology, which is the branch of the Pathology that is devoted to the study and diagnosis in tissue of hematological diseases. The diseases in which he is focused in both diagnosis and research are lymphomas.
When he is not working Dr Rosenwald likes sports, reading, ancient Greek archaeology and history
We wanted to talk to Dr Rosenwald today to ask him about the challenges ahead for research in his field of specialisation.
● Dr. Dr Rosenwald, you are internationally renowned in the field of lymphomas in terms of diagnosis and etiopathogenesis (mechanisms that lead to the development of a disease). Nowadays, how can we detect a lymphoma?
Lymphomas often lead to enlarged lymph nodes that will not decrease in size after initial treatment (e.g. antibiotic treatment). If there is a suspicion of lymphoma, an enlarged lymph node is usually excised surgically and sent to a pathologist with expertise in hematopathology. The hematopathologist uses histological, immunophenotypical (antibodies) and genetic techniques to render the diagnosis of lymphoma. It is important to determine the exact subtype of lymphoma, since they will be treated differently.
● Are the treatments for lymphomas currently changing according to the advances in the knowledge of their etiopathogenesis? Are they different depending on the type of lymphoma?
Absolutely. While multi-agent chemotherapy is still the backbone in the treatment of aggressive lymphomas, the addition of immunotherapy (e.g. using antibodies) has improved survival of lymphoma patients significantly. In more slowly growing lymphomas, strategies emerge to avoid chemotherapy at all by using more ‘biology-oriented’ drugs that inhibit certain signalling pathways that are aberrantly activated in these lymphomas.
● According to your studies, what mechanisms lead to the development of a disease, in this case lymphoma?
Lymphomas, like most of the other cancers, arise by the step-wise accumulation of genetic alterations in the genome of the tumor cells that lead to a growth advantage compared to neighboured, healthy cells. In lymphomas, some subtypes are associated with frequent genetic events – for example, almost all Burkitt lymphomas, a very aggressive subtype of B-cell lymphomas, carry a translocation of one of the most well known oncogenes (MYC oncogene) in the tumor cells that results in their abnormal high proliferation. The detection of this genetic alteration in the tumor cells is part of the diagnostic process in this lymphoma subtype.
● What progress has been made over recent years in this kind of disease?
With the improvement of immunochemotherapeutic approaches in many lymphoma subtypes, the survival of patients could be significantly improved over the last 10-15 years. In some lymphoma subtypes, the cure rate is now relatively high (e.g. Hodgkin lymphoma, diffuse large B-cell lymphomas). Some lymphomas that are not curable, but slowly growing can nowadays be converted into ‘chronic diseases’ and patients rather die with their lymphomas than from their lymphomas. However, there are still lymphomas (e.g. T-cell lymphomas) that have a terrible prognosis, and we need to learn more about the pathogenesis of these diseases to make progress in this field and to improve patients’ survival.
● In the talk you gave at the IJC you spoke about follicular lymphoma, which is the most common indolent non-Hodgkin’s lymphoma. What do we know today about this sub-type of lymphoma?
This is one of the lymphoma subtypes that – with modern and more biologically-oriented therapies – might be converted into ‘chronic diseases’. Some patients with this lymphoma subtype live with their lymphoma for 20-25 years. However, some patients with follicular lymphoma may show a rapid progression into an aggressive type of lymphoma and we need to learn more about the underlying basis of these cases. On the other hand, we have learned about some very indolent forms of follicular lymphoma that may not require any treatment at all. Thus, these patients could be spared a chemotherapy with all of the well-known side effects.
● Where is research into this kind of blood disease going?
As we understand more and more about the genetic basis and other aspects of the pathogenesis of lymphomas, we will be able to establish more precise and less toxic, more biologically oriented drugs that might have fewer side effects compared to standard chemotherapy. However, we also have to learn more about other aspects of the pathogenesis of lymphomas, e.g. about epigenetic changes and the interaction of the tumor cells with physiologic cells of our immune system.
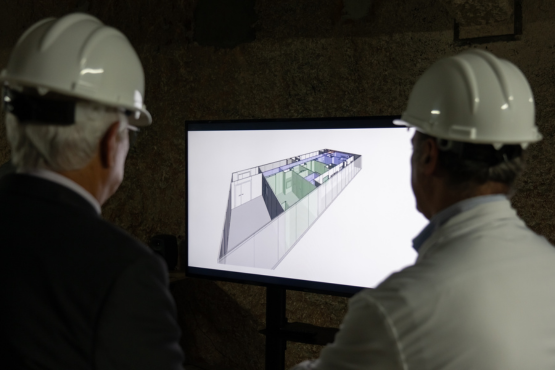
● The Josep Carreras Foundation has established a research centre specifically for leukaemia and other malignant blood diseases, the IJC. What do you think the repercussions of this will be, both for medical science and for society at large?
Hematological diseases have always been at the forefront of cancer research in general – many aspects that have been initially identified in hematological cancers are now also being studied in other types of cancer. During my visit at the IJC I was very impressed by the high quality of research that is being performed there. The new research building that will be inaugurated in 2017, will certainly boost the research efforts at this beautifully located place in Badalona (I would love to work in such a great ‘ambiente’!). Thus, lymphoma and leukemia research, but also the society at large will benefit from the enormous efforts that are being undertaken at the IJC!