Leukaemia, bone marrow and blood cells
Leukaemia is a type of blood cancer that originates in the blood cells that are located in the bone marrow. There are many different types of leukaemia that can affect both children and adults. Each type of leukaemia can affect one cell group and has different treatments and prognoses. In general, we speak of acute leukaemias for those with an aggressive course, and chronic leukaemias, whose affected cells proliferate slowly.
 Leukaemia causes an uncontrolled increase in white blood cells. These cancer cells infiltrate the bone marrow and prevent the rest of the blood cells (healthy red blood cells, platelets and white blood cells – leukocytes) from forming properly.
Leukaemia causes an uncontrolled increase in white blood cells. These cancer cells infiltrate the bone marrow and prevent the rest of the blood cells (healthy red blood cells, platelets and white blood cells – leukocytes) from forming properly.
Thus, among others, leukaemias involve characteristic symptoms of anaemia, due to poor red blood cell production; haemorrhages or petechiae, due to insufficient or dysfunctional creation of platelets; and susceptibility to infections, due to lowered defences (lymphocytes).
In Spain, according to data from the SEOM (Spanish Society of Medical Oncology), around 6,000 new cases of leukaemia are diagnosed each year. Of these, about 350 cases are children. Leukaemia is the most common cancer in the paediatric age group, as 30% of the neoplasms diagnosed in children are leukaemias.
Leukaemia is not the only blood cancer. In fact, it is not the most common either. In Spain, more than 10,000 different lymphomas, more than 3,000 cases of multiple myeloma and around 3,000 myelodysplastic syndromes are diagnosed each year.
Recommended materials:
What is leukaemia? Ted Lessons. Danilo Alegra and Dania Puggioni
Marrow: the factory of life. Dr. Helena Alves. Portugal.
The bone marrow is the body’s ‘blood factory’.
Bone marrow is a spongy tissue found inside some of the bones of the body such as the iliac crests (hip bone), the sternum or the bones forming the skull. In colloquial language it is called marrow. It should not be mistaken for the spinal cord as they have nothing to do with each other. Their functions are totally different. The spinal cord is located in the spinal column and transmits nerve impulses from the brain to the entire body and vice versa.
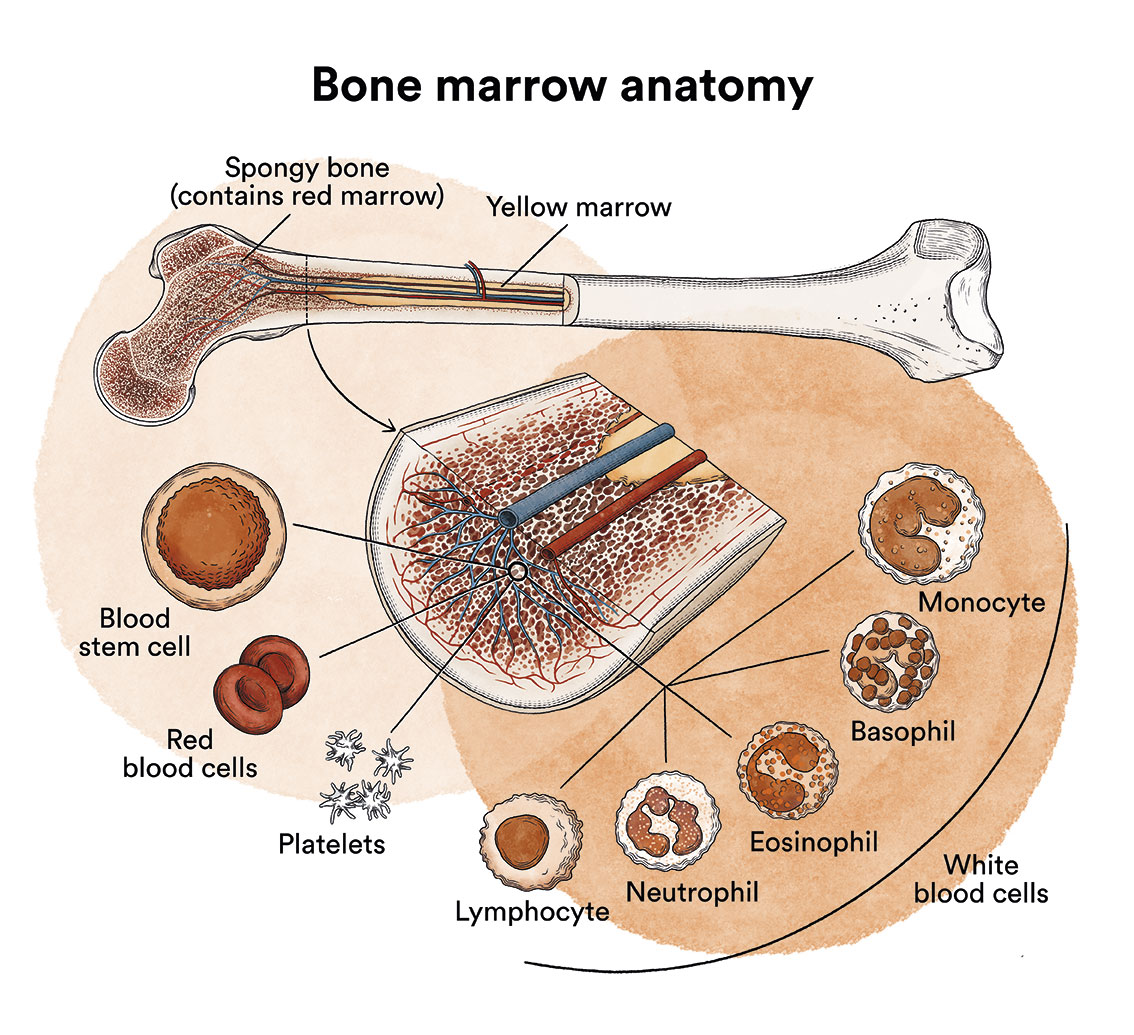
Bone marrow contains immature cells called blood stem cells (haematopoietic stem cells) that divide to create more cells which then give rise to all the cells in the blood, the three most important of which are: white blood cells that defend us from infection; red blood cells that carry oxygen in the body; and platelets that help the blood to clot.
The blood stem cells of a healthy person can be transplanted in some cases to treat acute leukaemias, aggressive lymphomas or in patients who do not respond well to treatments.
See Bone marrow, peripheral blood or umbilical cord blood transplantation
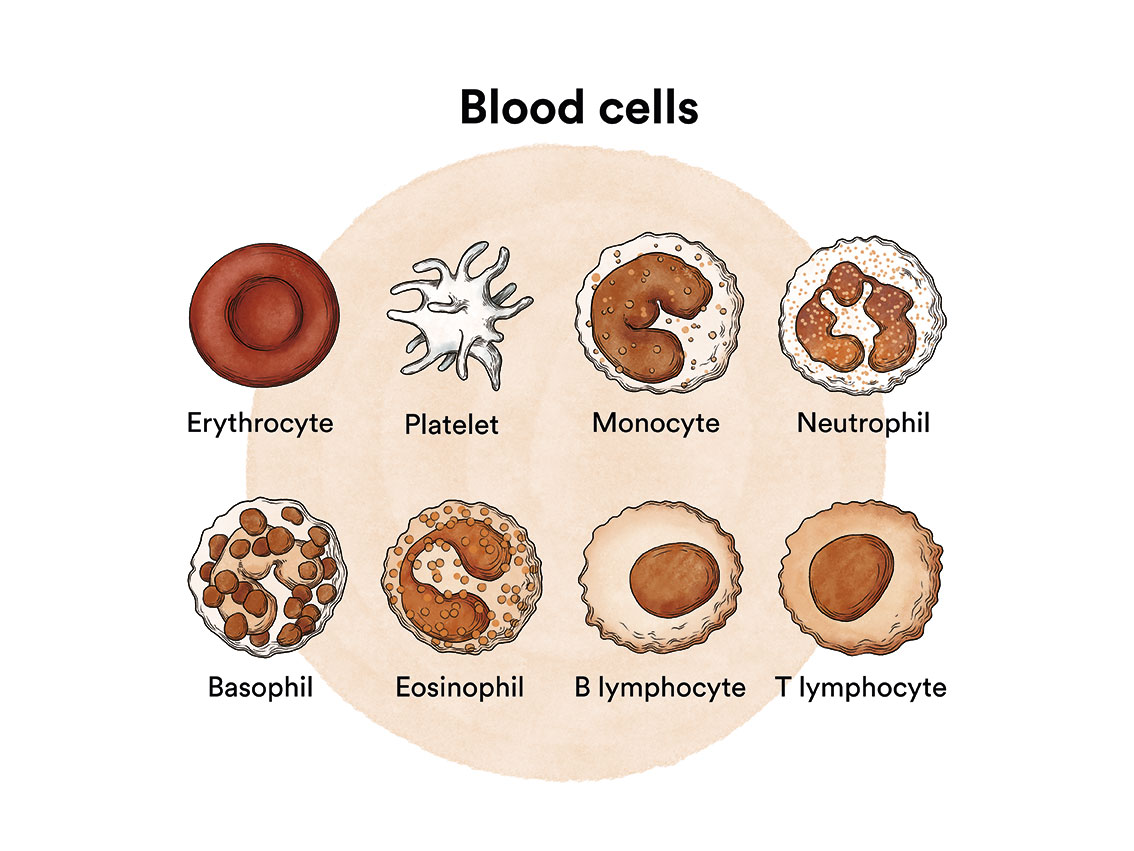
Blood is made up of a fluid called plasma and three major types of cells, each of which has a specific function.
The red blood cells, also called haematids or erythrocytes, are the cells responsible for transporting oxygen from the lungs to the tissues, and for carrying carbon dioxide from the tissues back to the lungs for expulsion. Like other blood cells, they are produced in the bone marrow. Red blood cells give blood its characteristic red colour. The red blood cell count can be assessed in blood tests. Anaemia occurs when the body’s red blood cell levels are below normal. When there are insufficient red blood cells, parts of the body do not receive sufficient oxygen and, as a result, cannot function as they should, thus leading to problems. In a healthy organism, hundreds of billions of red blood cells are produced every day!
White blood cells or leukocytes are the body’s defence against infection and foreign substances that may enter the body. To defend the body properly, there needs to be a sufficient number of white blood cells capable of responding adequately, reaching the place where they are needed, and then destroying and digesting harmful micro-organisms and substances. Like all blood cells, white blood cells are produced in the bone marrow. They are formed from precursor cells (stem cells) that mature into one of the five main types of white blood cells: neutrophils, lymphocytes, monocytes, eosinophils and basophils. A person produces approximately 100 billion white blood cells per day. If white blood cell production decreases, the patient is more prone to infections.
Platelets or thrombocytes help blood to clot when a blood vessel ruptures. They help produce blood clots to slow or stop bleeding and to facilitate wound healing. When the amount of platelets is insufficient, the blood cannot clot as it should, resulting in an increased risk of bleeding. This situation is known as thrombocytopaenia. In this situation, bruising or petechiae may also form. Thrombocytopaenia means that you have fewer than 150,000 platelets per microlitre of circulating blood. Because each platelet lives for around 10 days only, your body normally renews its supply of platelets continuously by producing new platelets in the bone marrow.
All blood cells in the bone marrow are the result of differentiation and maturation of stem cells, and are often collectively referred to as haematopoietic progenitors.
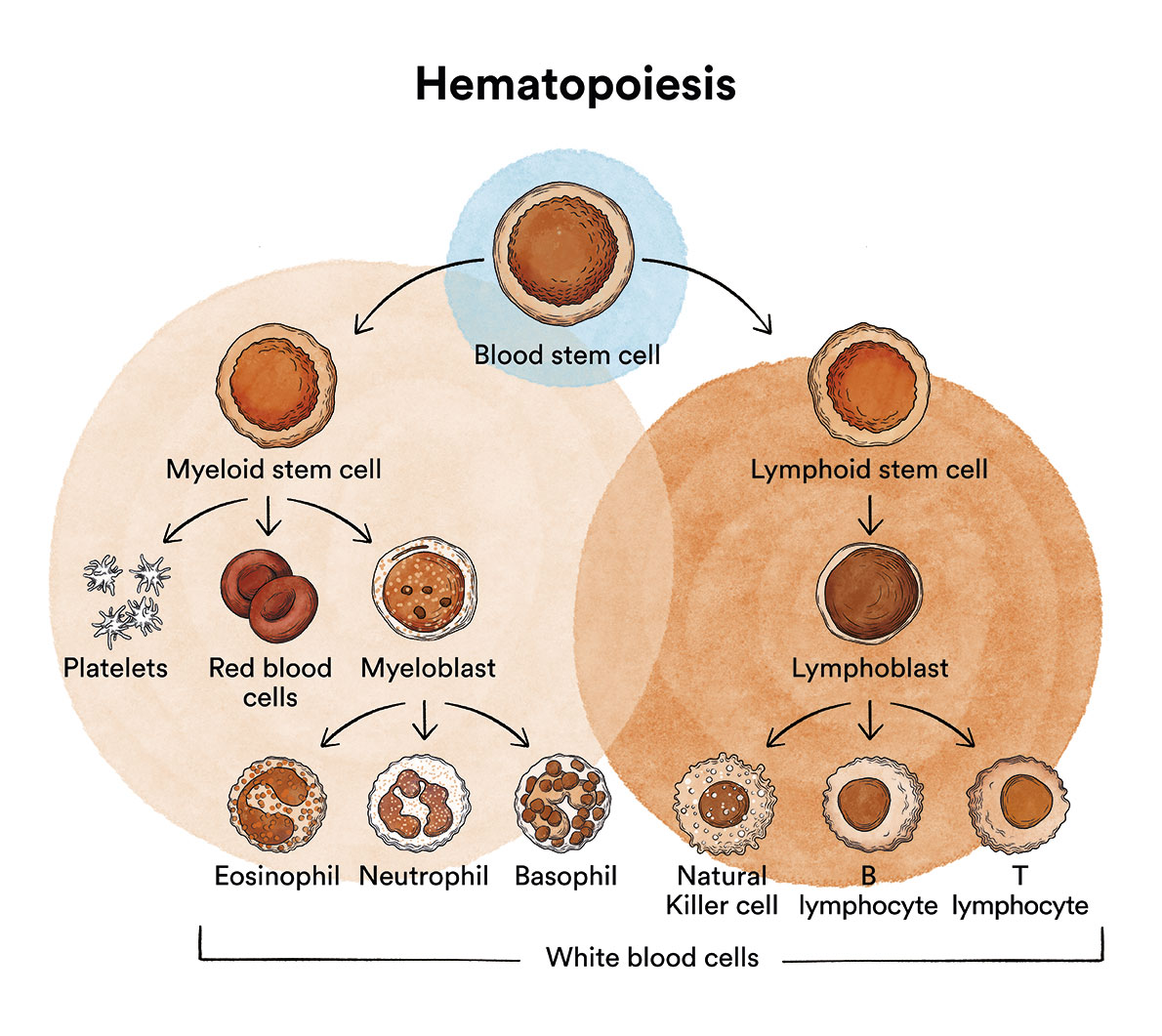
Under normal conditions, the production of blood cells takes place in a controlled manner, as the body needs them. The alteration of this balance can lead to various diseases; some are due to an insufficient production of all blood cells (marrow aplasia) or of a specific type of blood cell (erythroblastopaenia, amegakaryocytosis, agranulocytosis); others are caused by the production of cells incapable of carrying out their own functions and in insufficient quantities (myelodysplastic syndromes) and finally, others are due to the production of cancer cells in large numbers (leukaemias, thrombocythaemia or polycythaemia).
Despite all the advances and relentless research, the causes of leukaemia remain unknown. The incidence is known to be higher in males than in females, and in terms of race, white people have a greater prevalence than black people. However, it is not yet possible to provide a satisfactory explanation as to why some people develop the disease while others do not.
Through the study of a large number of cases, it has been possible to establish certain risk factors that may favour the development of this disorder. For example, exposure to large doses of high-energy radiation, such as from the atomic bomb explosions in Japan during World War II, or from accidents at nuclear power plants, increases the risk of developing leukaemia. Therefore, in nuclear power plants, strict safety standards are in place to protect workers and the public from exposure to harmful radiation. In contrast, no correlation has ever been found between electromagnetic radiation (mobile phones, telephone and radio antennas, etc.) and the development of leukaemia.

Some genetic characteristics may increase the risk of developing leukaemia. One of these characteristics are Down syndrome, Li-Fraumeni syndrome or Fanconi anaemia. Children born with these syndromes are more susceptible to the disease.
Furthermore, exposure to certain chemicals, such as benzene, over long periods of time may also be a risk factor. Treatments used to fight other types of cancer can also increase the patient’s risk of developing leukaemia. However, the latter factor represents a minimal risk compared to the benefits of chemotherapy.
As scientific research into leukaemia continues, new and better ways of treatment are being discovered and the chances of a cure continue to increase. Nevertheless, it is normal for both patients and their families to be concerned about the future.
With the aim of one day making leukaemia a 100% curable disease and to improve the quality of life of patients, in 2010 the Josep Carreras Foundation launched the Josep Carreras Leukaemia Research Institute. This Institute is the first in Spain to carry out research exclusively on haematological malignancies and one of the largest centres of its kind in Europe.
Survival averages and other statistics are sometimes used to try to elucidate whether a given patient will be able to overcome the disease. However, it is important to remember that statistics and averages are calculated over a large number of cases and cannot be used to predict the evolution of a specific patient, as no two patients are the same, and responses to treatment can vary greatly from one patient to another. Thus, cure rates can range from 90% in certain types of acute myeloblastic leukaemia (promyelocytic leukaemia) or acute lymphoblastic leukaemias in children, to less than 20% in leukaemias occurring after myelodysplastic syndrome or the acute phases of chronic myeloid leukaemia. It is the haematologist in charge of the patient who is in the best position to give an opinion on the prognosis, but always bearing in mind that even the former may not know what the outcome will be.
Cancer outcomes are usually described in terms of how many people survived 5 years after diagnosis and treatment. This is why it is common to read “5-year survival”. This concept does not mean that the patient will live 5 years, but rather the percentage of patients who according to studies lived 5 years or more. Of course many people live much longer than 5 years after remission, although most cancer relapses appear within 5 years after treatment has ended. If the patient has been in remission for 5 years or more, it is unlikely the cancer will return.
Doctors often speak of survival, or remission rather than cure, since the disease may recur in some cured leukaemic patients. A complete remission occurs when the leukaemia is undetectable in the body and there are no symptoms. This may also be referred to as “no evidence of disease” (NED). In the case of partial remission, this means that some signs and symptoms of the cancer have disappeared, but not all of them.
DNA (deoxyribonucleic acid) is a complex protein found in the nucleus of every cell in our body. This is information that is inherited in living beings. Almost every cell in the body has the same DNA code. The order and sequence of this code determines all the information the organism needs to form and maintain a healthy condition. Like the alphabet, their order and composition can form letters, words and sentences.
An important property of DNA is that it can replicate or make copies of itself. Each strand of DNA in the double helix can serve as a template for duplicating the sequence of bases. This is essential when cells divide, because each new cell needs to have an exact copy of the DNA present in the original cell. The DNA inside each cell is in long strands called chromosomes. Every time a cell divides into two new cells, it has to make a new copy of its chromosomes. This process is not perfect and errors can occur, such errors affect the genes contained in the chromosomes.

A gene is the unit of information at a locus (fixed position on a chromosome) in the DNA. Genes are small pieces of DNA. Genes influence a person’s risk of developing some diseases and conditions. Each of us has around 24,000 different types of genes.
Genes that help cells to grow, divide or stay alive are called oncogenes. Genes that help maintain control of cell division or cause cells to die at the right time are called tumour suppressor genes.
There are several types of chromosome changes that can be found in the cells of some types of leukaemia:
- Translocations are the most common types of chromosomal changes. It means that a part of one chromosome breaks off and attaches to a different chromosome. At the point of this detachment, genes can be activated or deactivated. As if a part of a book in a library were to attach itself to another book.
- Deletions occur when part of a chromosome has been lost. In this loss, a gene that helped keep cell growth in check may no longer be present. As if a part of a book were to have been lost.
- Inversions occur when a part of the chromosome is presented, but in an inverted order. It can also cause the loss of a gene because the cell can no longer read its instructions. As if a book were upside down in a library.
- A duplication or addition occurs when there is a copy of part or all of a chromosome. This can lead to the generation of too many copies of a gene within a cell. As if there were several repeated chapters within a book.
Leukaemia can develop when there is a mutation in the DNA of a blood cell. A mutation is a change in one or more genes. The mutation may be due to one or more DNA changes, a change in many genes, the loss of one or more genes, or the rearrangement of genes or entire chromosomes. The body can repair many mutations that occur in our body’s everyday life. However, in leukaemia, this mutation disables the body’s ability to control cell growth and division. As a result, mutated and immature cells grow out of control, invade the bone marrow and crowd out healthy cells in the bloodstream.
Although leukaemia is not an inherited disease, some children may inherit DNA mutations from a parent. This increases the risk of developing cancer. However, these inherited mutations are not the cause of most leukaemias in children. In these cases it is a genetic factor, with a hereditary predisposition to the disease.
Most leukaemia-related DNA mutations usually develop after conception. Some may even occur during gestation, before birth. They are therefore acquired genetic mutations and are exceptional.
In adults, most DNA changes occur during a person’s lifetime and are not inherited from birth. Many of these genetic changes are probably just random events that sometimes occur inside a cell, with no apparent cause. They seem to occur more frequently as we get older. Therefore, we could say that cancer in children is a disease related to growth, whereas cancer in adults is a disease related to cell ageing.

Miranda, 22 years old
Acute Myeloid Leukaemia.
“On August 13, 2020, I was diagnosed with acute myeloid leukaemia. I was 19 years old. It was a hardship for both me and my family. In 2021 I had a bone marrow transplant. I must admit that I was very afraid. There are many days away from home, away from mine. I have had many complications, but I am grateful to all the professionals for getting me out of the worst and helping me so much. Thank you. I only have words of gratitude.”


