“Treatment for patients with MDS is becoming more and more personalised. In the coming years we are going to see more emphasis on the genetic mutations associated with MDS. Every patient has a different pattern of mutations and these mutations can be used to indicate how the patient should be treated. The mutations can be used to establish the diagnosis, determine the prognosis and to predict which therapies will be the most efficacious.”
Today it is our great pleasure to welcome Dr. Rafael Béjar to the Catalan Institute for Oncology/Germans Trias i Pujol Campus of the Josep Carreras Leukaemia Research Institute (IJC).Dr. Rafael Béjar is an internationally renowned expert in the study of myelodysplastic syndromes (MDS) and works at the University of California, San Diego, where he has set up a centre of excellence in this field based on bringing together the best diagnostic tools, health-care practice, clinical trials and medical experience under the same roof.
On 8 March Dr. Béjar gave a talk at our centre.
As well as tending to patients, Dr. Rafael Béjar carries out scientific research programmes focussed on the study of myelodysplastic syndromes to discover which of the disease’s characteristics can be used to personalise treatment for patients, the aim being both to prolong life and to find a cure.
He has published key articles in the New England Journal and the Journal of Clinical Oncology in which he examines the genetic changes that lead to the development of MDS. His efforts have led to the development of clinical trials with mutations that help formulate a prognosis and which assist in the choice of individualised treatments for patients.
Dr. Béjar finished his medical internship at the Brigham and Women’s Hospital in Boston where he later held a number of senior posts. He was awarded a grant for hematology and oncology at the highly renowned Dana–Farber Cancer Institute. Having graduated as a doctor he undertook his doctoral studies at the University of California, San Diego.
When he’s not working Dr. Béjar likes to spend time with his wife and three children. He’s also a keen cyclist and he likes diving off the San Diego coastline.
We wanted to ask Dr. Béjar more about current challenges in the field of research into myelodysplastic syndromes.
● Prof. Béjar, what does a diagnosis of MDS mean these days and what kind of patients are affected?
Myelodysplastic syndromes are diseases typically found in older patients. They cause cytopenia and can lead to acute leukaemia. Patients with MDS have many different symptoms. Those at low risk might have few symptoms and not be affected for many years. Others, however, need blood transfusions. High-risk patients have more severe cytopenia and need more regular transfusions. It is probable that for such patients the disease will lead to acute leukaemia, requiring more aggressive treatment.
● How were patients with MDS treated 25 years ago and how are they treated now?
The treatment for these diseases has changed a lot over the last 15 years. Before, we were only able to provide supportive therapy to our patients. Such treatment included blood transfusions, platelet transfusions and growth factors for red blood cells. None of these procedures treated the disease directly. Some patients may have received a bone marrow transplant, but the vast majority of patients were not good candidates for this kind of intensive treatment.
Twelve years ago three new treatments were approved for MDS: lenalidomide, azacitidine and decitabine. These drugs act on the disease directly and can lengthen the lives of those patients who respond to treatment.
Treatment for MDS today is highly individualised. Each patient is asessed to determine their prognosis. Low-risk patients receive treatment to improve their quality of life, and high-risk patients are treated with aggressive therapies with the aim of prolonging life. Bone marrow transplants have improved over the last 25 years and these too are considered for high-risk patients.
● It is the case, is it not, that challenges for the future involve new strategies for personalised treatment? What aims have been set for the coming years?
That is true. Treatment for patients with MDS is becoming more and more personalised. In the coming years we are going to see more emphasis on the genetic mutations associated with MDS. Every patient has a different pattern of mutations and these mutations can be used to indicate how the patient should be treated. The mutations can be used to establish the diagnosis, determine the prognosis and to predict which therapies will be the most efficacious. At the same time there are many new treatments in clinical development.
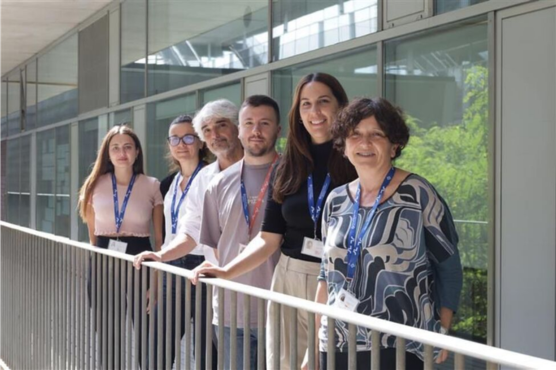
Dr. Bejar with Dr. Francesc Solé, scientific director of the ICO-Germans Trias i Pujol Campus of the IJC and director of myelodysplastic syndromes research group and Vera Ademà, IJC myelodysplastic syndromes group researcher.
● Over recent years, thanks to research, new biological agents such as lenalidomide and azacitidine have appeared and these provide new opportunities for elderly MDS patients who can not undergo a bone marrow transplant. Can you tell us about the importance of these new biological agents and whether new studies are taking place with other treatments?
These new treatments can improve cytopenia and prolong life. Unfortunately they do not cure MDS. Some patients do not respond to these treatments and relapse is common. New and more efficacious treatments are needed. Fortunately, at present, various new treatments are being developed or are at the clinical trials phase. These treatments can complement our already established treatments, or might replace them. Furthermore, bone marrow transplants have improved a great deal. Elderly or very weak patients in a poor state of health might now be considered as candidates. Moreover, patients who no not have a donor within the family now have greater possibilities of receiving a bone marrow transplant from a non-related donor.
● Do you think that in the future MDS will be considered a chronic disease?
For low-risk patients MDS can already be considered a chronic disease. I think that with new treatments these patients are going to have a much better quality of life or, ideally, a totally asymptomatic disease. I hope that treatments for high-risk patients will generate profound and long-lasting remission and prevent the transition to acute leukaemia. At least it would be an important step forward to have various treatments available for these patients so as to still have some options open when the first line of treatment either fails to work or stops working. This would help to prolong the lives of high-risk MDS patients more successfully than we can today.
● Myelodysplastic syndromes are not rare but people do not know much about them. What are your thoughts about the Josep Carreras Foundation having established a specific research centre for leukaemia and other malignant blood diseases such as MDS? What do you think the likely repercussions will be, both in the scientific world, as well as for society in general?
It is true that people do not know a lot about MDS and it is of great importance that the Josep Carreras Foundation has set up a research centre for MDS and related diseases.
The fact that there are world-class researchers working on MDS in Spain means that the society in which they are working will become aware of these diseases.
Furthermore, doctors will be better informed and there will be greater opportunity to educate people about these diseases that are commonly found in the elderly. Both patients and doctors will be more aware of what MDS are and doctors will be better placed to diagnose and treat them correctly. Greater public awareness means greater public defence and more support from governments and other sources of funding for future research.
Thank you very much!