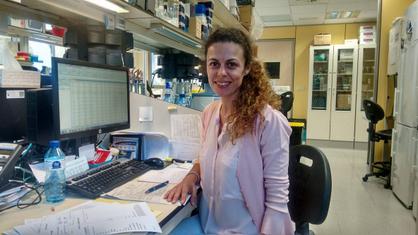
Dr Maria Joao Baptista
She’s a researcher from the Josep Carrreras Leukaemia Research Institute (Campus ICO-GTiP)
Age: 41
Place of birth: Porto (Portugal)
Mini curriculum
I studied pharmacy in Porto and I was an Erasmus student in Madrid, the first Spanish city I lived in. I went back to Porto and did a Master’s degree in oncology and started working in the field of hematology. Having finished my dissertation I did a doctoral course in Salamanca under the supervision of Prof. Alberto Orfao. I moved to Barcelona in October 2005 to write my doctoral thesis under the supervision of Prof. Emili Montserrat and Dr. Francesc Bosch at the Hospital Clínic. At that time I devoted my full attention to research into B-cell lymphoproliferative syndromes.
It was just when the practical part of my thesis was drawing to an end that I started working at the Josep Carreras Leukaemia Research Institute. It was difficult to start off with because I was writing my thesis and, at the same time, I had embarked on this great IJC project. I was one of the first researchers at the Institute and that is something I’m very pleased about. I very much appreciate the IJC’s confidence in me and I very much hope to be able to fulfil expectations!
4 words to define you:
Persistent, methodical, demanding, creative.
– You have recently published a scientific paper entitled, “Homeobox NKX2-3 promotes marginal-zone lymphomagenesis by activating B-cell receptor signalling and shaping lymphocyte dynamics”. What is it about?
The paper is about a study of the role of the NKX2-3 protein in the development of lymphomas. It all started upon the observation that some patients with marginal zone lymphoma express NKX2-3 in an augmented way. Transgenic mice are produced that express NKX2-3 and it can be observed that these mice develop tumours similar to those of patients with marginal zone lymphoma. It is therefore thought that the overexpression of the NKX2-3 protein might play an important role in the appearance of these lymphomas. To reveal the role of the NKX2-3 protein in the development of these lymphomas various experiments have been undertaken, from which it can be concluded that NKX2-3 induces B-cell receptor pathway signalling, and they have also made it possible to identify the various proteins involved in the process and their respective effects on survival, proliferation and migration.
– Could you tell us, in terms a layman can understand, about the research you are doing at the IJC?
There are a number of projects underway in our group and almost all of them are focused on aggressive lymphomas in patients with HIV. These patients present a greater incidence of lymphomas than the rest of the population on account of HIV depressing the immune system. From the hematological point of view it is possible, at the present time, to treat these patients in the same way as patients who are not infected with HIV and the responses to treatment for the lymphoma are identical. However, as occurs with patients who are not infected with HIV, there are some who do not respond to standard treatments, and others whose response is short-lived. Furthermore, lymphomas in patients with HIV tend to be more aggressive and, at the biological level, the tumour cells are exposed to other factors. In the lymphoid neoplasia group we are looking for markers that will enable us to identify patients that might not respond to standard treatments, or have only short-lived responses. We are also trying to understand the differences there are between patients who are infected with HIV and those who are not.
– Why did you focus on the study of lymphomas?
I suppose I could say it happened by chance. The first research work I did, when I was doing my Master’s in oncology, was the study of T lymphocyte and NK cells. When I was in Salamanca I started studying lymphoproliferative syndromes, and lymphomas are in this group of hematological diseases. From there, my doctoral thesis and my work at the IJC have continued along those lines.
– Let us assume that a 41-year-old-woman is diagnosed as having diffuse large B-cell non-Hodgkin lymphoma and that she is also infected with HIV. What is the difference between her being diagnosed today in comparison with what would have been the diagnosis 25 years ago?
The HIV virus was only discovered 33 years ago (1983) so 25 years ago the treatments available for HIV were not very effective and patients with HIV did not have a very long life expectancy. At that time attention was focused on combating HIV rather than on the lymphoma. HIV was a devastating disease and when a lymphoma was diagnosed in such patients their general condition was a very delicate one. When possible, chemotherapy was applied for the lymphoma but the associated complications were very frequent and this led to the dosage being reduced and long pauses between cycles of treatment. The results obtained were correspondingly disappointing. In this regard we must applaud the progress that has been made in research into HIV, thanks to which, these days, patients infected with HIV are treated in the same way as patients who are not infected.
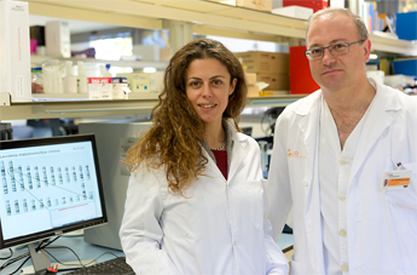
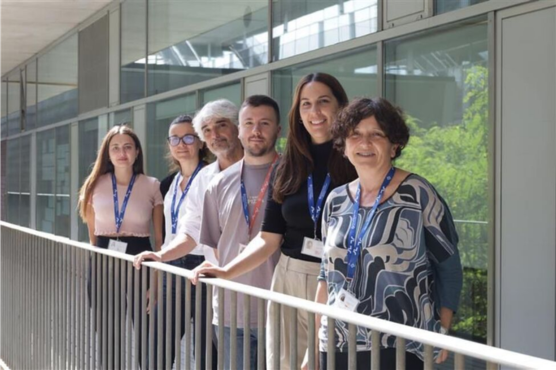
Dr. Maria Joao with Dr. Tomás Navarro, lead researcher at the IJC lymphoid neoplasms research group.
– How would you describe a research centre like the IJC? Why is it interesting?
The IJC is a centre specifically for research into leukaemia. As such, it is quite unique in the world. There are great advantages in bringing different researchers together, all of them devoted to the study of different kinds of leukaemia and other malignant blood diseases, because it facilitates the exchange of information and experience. The IJC has other interesting aspects, the fact, for example, that it is spread over three campuses, each of which is near a major hospital.
– What is your working day like?
I think I spend my days like most of my colleagues. There isn’t much time for activities outside the world of work. Basically I spend my time in the laboratory.
– What do you most and least like about your work?
What I most like about my work is being able to study and to be constantly learning. Every day is a challenge and there is something new all the time. Routine is something that does not exist in the life of a researcher.
What I least like is the way in which research is funded and the way it is regarded by society. Everyone recognises the effort involved, but the life of a researcher is a precarious one. Society comforts itself by thinking our work is a vocation. Yes, it is a vocation, like many others, but that does not mean that we have to do our work, develop our projects and eke a living on the basis of grants.
I spend a great deal of my time in summarising projects for calls to tender for grants, filling in forms, ticking boxes. There is a great deal of bureaucracy involved in the whole process and it is a difficult process because the percentage of projects that are awarded funding is a small one.