“It was an excellent idea to build up a special center dedicated to leukaemia and related disorders here in Barcelona. This center is collaborating with international research partners. The exchange to knowledge, techniques and ideas and the development of study protocols and projects with cooperating partners has tremendous impact on scientific progress”.
Today we have the great pleasure of greeting, here at the Josep Carreras Leukaemia Research Institute ICO-Germans Trias i Pujol Campus, Prof. Ulrich Germing, world known expert in the study of myelodysplastic syndromes (MDS) who carries out his work at Düsseldorf University Hospital (Germany). Prof. Germing is giving a lecture at our centre this morning.
Prof. Germing is vice head of the department of Hematology, Oncology and clinical immunology, University clinic, Heinrich-Heine-University Düsseldorf. He studied medicine from 1986 to 1992 and became member of the MDS working group in 1989, being responsible for the MDS registry. In 1998 he passed the board certification in Internal medicine, in 2001 in Hematology and Oncology. Since 1999 he is head of the MDS working group and since 2007 he is member of the clinical advisory committee of the WHO for the classification of myeloid and lymphoid malignanicies. Prof. Germing is married and has two sons.
We are very happy to be able to talk to Prof. Germing for we have many bonds that connect us to him and his environment. Historically, the Josep Carreras Foundation has an “almost sentimental” bond with the city of Düsseldorf, for it is there where our German Foundation created its first and main umbilical cord blood bank in Germany, the José Carreras Stammzellbank, in 1992. It was one of the oldest cord stem cell blood banks in the world. Also, at the IJC we have a very active specific research line on myelodysplastic syndromes directed by Dr Francesc Solé. And, on the other hand, Dr Blanca Xicoy, haematologist at the Catalan Oncology Institute (ICO-Germans Trias I Pujol) and researcher at the IJC was working during 2014 with Prof. Germing in Düsselforf, focussing their interest on the clinical study and treatment of MDS patients in the Düsseldorf MDS registry he directs in our sister city.
Today, we wanted to talk to Prof. Ulrich Germing so he could explain a little more about the current challenges in myelodysplastic syndrome research.
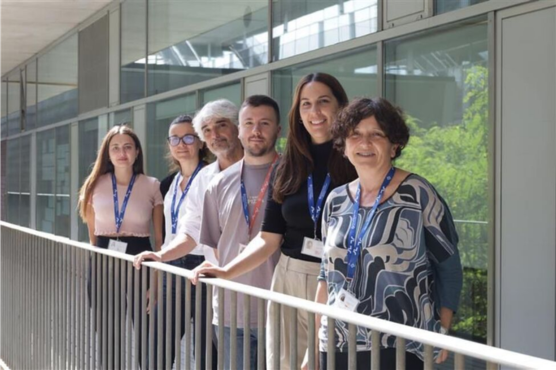
From left to right: Dr. Francesc Solé, scientific director of the ICO-Germans Trias i Pujol Campus of the Josep Carreras Leukaemia Research Institute (IJC); Prof. Evarist Feliu, vice president of the José Carreras Foundation and director of the Board of the IJC; Prof. Ulrich Germing; Dra. Blanca Xicoy, Dr. Josep Mª Ribera and Dr. Tomas Navarro, members of the medical team of the Catalan Institute of Oncology in Badalona and researchers of the IJC.
● Prof. Germing, you direct one of the oldest and most active MDS patient registries. Why is the preservation and analysis of samples of a heterogeneous group of diseases such as MDS essential?
When Prof Aul started the registry in 1982 when the FAB classification came out, established. Prof. Aul developed a standardized way to describe blood and marrow cells and the dysplastic signs. Every patient who was diagnosed with MDS in our lab was entered into the registry and followed up. The growing amount of data allowed epidemiologic, diagnostic, prognostic and therapeutic analyses. An exact diagnosis and good description of the clinical course of the disease is essential in order to better define homogeneous subgroup within the very heterogeneous entire group of MDS patients.
● Study of the samples obtained at a bio-bank such as the one you direct has shed light on the prognosis of these diseases in the last few years. Future challenges involve development and, above all, new treatment strategies. Is this so? What are the goals for the next few years?
When we subsequently built up a biobanking linked to the registry it was possible to perform lab analyses such as cytogenetics, gene arrays, proteomics, and stroma examination on material of well documented patients. Of course the most important driver for scientific approaches always is the aim to offer treatment to the patients. The problem is the lack of predictive markers that allow to better offer specific treatment in a “personalized” way. MDS researchers should therefore conduct clinical trials accompanied by lab research in order to identify predictive markers. In addition new compounds are to be examined in clinical trials.
● In the last few years, through research, new biological agents such as lenalidomide or azacitidine have come up, giving new chances to MDS patients, especially older ones who cannot go through a bone marrow transplant. Can you explain what this type of biological agents suppose and if there are new on-going studies on other treatments?
There are different problems related to the new drugs in MDS: it is not known how the immunmodulators and hypomethylating agents work. Several sorts of drug activities have been described, probably more than one mode of actions play a role. We know that lenalidomide is helpful in the majority of patients with MDS del(5q), but we do not know, what patients respond to hypomethylating agents. About the half of the patients get treated in vain. In addition, almost all responders relapse. As a result, there is a large gap and a high medical need for non responders. Most importantly no drug has been approved for the majority of patients. When looking back on the last two decades, many clinical trials failed. New ongoing clinical trials are aiming at niches, but seem not to be breakthroughs.
● What future could personalised medicine have for myelodysplastic syndromes?
The myelodysplastic syndromes could be a perfect example for the need for personalised treatment: they are extremely heterogeneous with regard to clinical course, genetic and epigenetic characteristics and no single type of treatment is effective in all patients. Unfortunately it will take some time to develop personalized treatments in MDS, as high troughput techniques until now did not detect information that had direct impact on the choice of treatment.
Members of the MDS Group Düsseldorf: Ulrike Spiegelberg, Study nurse, Dr. Michael Wulfert, Biobanking, Jennifer Schemenau, MDS Registry, Ulrich Germing
● The worst prognosis for MDS patients are for those who have a high risk of becoming acute myeloid leukaemia. Do you think we will witness a future “revolution” for this kind of MDS that will help us to make the disease chronic?
High risk MDS patients regardless if they develop acute leukemia or not are facing a desastrous prognosis. Even after allogeneic stem cell transplantation the relapse rate is high. To be honest, I do not see a therapeutic revolution for these patients leading to a chronic disease.
● On occasion, myelodysplastic syndromes appear as a secondary disorder associated to radiotherapy or chemotherapy administration to a patient suffering from a previous neoplasm. What studies are being done in order to control or prevent these secondary diseases from appearing?
It is a pitty that virtually all clinical trials exclude therapy-associated MDS. We should be aware that this patient group is slowly growing as more and more patients survive a primary malignancy and later are at risk to develop a myeloid malignany such as MDS. Some lymphoma and myeloma study groups, such as ours, monitor patients very carefully in order to early detect signs for secondary diseases.
● Myelodysplastic syndromes are not strange diseases but they are not well known to society. What is you opinion on the Josep Carreras Foundation having created a specific research centre for leukaemia and other haematologic diseases such as MDS? How do you think it can impact both the scientific world and society?
Indeed the Myelodysplastic syndromes are not well know in the society, probably because the diseases usually do not present spectacularly but rather smoldering and because the vast majority of the patients are old. It was an excellent idea to build up a special center dedicated to leukaemia and related disorders here in Barcelona. This center is collaborating with international research partners. The exchange to knowledge, techniques and ideas and the development of study protocols and projects with cooperating partners has tremendous impact on scientific progress. A good example for a fruitful collaboration took place in 2013/14 when Dr. Blanca Xicoy spent a year in Düsseldorf, inspiring myself and our group. Josep Carreras foundation is extremely well known and can help to publicize the complexity of the disease and the important medical need for the patients.
Thank you very much!