Burkitt lymphoma in children and teenagers
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.

Francesc
Burkitt's lymphoma.
“In 2011 Francesc, only 4 years old, was diagnosed with Burkitt’s lymphoma, a cancer of the lymphatic system that was very aggressive but responded well to chemotherapy, according to what the doctors told us at the time. The initial uncertainty gave way to the courage to face a tough, short but effective treatment. We spent a different summer in the hospital, with very strong chemotherapy protocols, but also very effective in eliminating the ‘bad bugs’. We have seen a lot of suffering in the hospital. We are very grateful! We have felt the passing of time, we have learned to enjoy the little things, we have learned to value life!”.
Information endorsed by… ![]()
Information reviewed by Dr. Rocío Parody Porras, Doctor specialising in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
What is Burkitt lymphoma in children and teenagers and who does it affect?
 Burkitt lymphoma, also known as small noncleaved cell lymphoma, is a type of aggressive non-Hodgkin’s lymphoma that mainly affects children, adolescents and young adults. Generally speaking, it is most frequent in males aged between 5 and 10 years old. There are three main types of Burkitt lymphoma: sporadic, endemic and immunodeficiency-related, Sporadic Burkitt lymphoma is present around the world, endemic Burkitt lymphoma is present in central Africa, and immunodeficiency-related Burkitt lymphoma is most frequently observed in those infected with HIV. Some forms of Burkitt lymphoma are related to the Epstein-Barr virus. It is named after the doctor Denis Parsons Burkitt, who described this disease when working in Equatorial Africa in 1956.
Burkitt lymphoma, also known as small noncleaved cell lymphoma, is a type of aggressive non-Hodgkin’s lymphoma that mainly affects children, adolescents and young adults. Generally speaking, it is most frequent in males aged between 5 and 10 years old. There are three main types of Burkitt lymphoma: sporadic, endemic and immunodeficiency-related, Sporadic Burkitt lymphoma is present around the world, endemic Burkitt lymphoma is present in central Africa, and immunodeficiency-related Burkitt lymphoma is most frequently observed in those infected with HIV. Some forms of Burkitt lymphoma are related to the Epstein-Barr virus. It is named after the doctor Denis Parsons Burkitt, who described this disease when working in Equatorial Africa in 1956.
- The sporadic variant of Burkitt lymphoma (also known as the non-African variant) is associated with an infection caused by the Epstein-Barr virus.
- The endemic (or African) variant of Burkitt lymphoma occurs in equatorial or central Africa. It is the most frequently diagnosed type of cancer in children in this part of the world. In general, these children also have a chronic malaria infection and it is thought that this could perhaps be the reason for a decrease in resistance to the Epstein-Barr virus. African children tend to develop this lymphoma in the jaw or other facial bones.
- The immunodeficiency-related variant of Burkitt lymphoma is particularly linked to the HIV virus or as a result of an immunodeficiency caused by a previous transplant or in cases where the patient is taking immunosuppressant medications.
What are the causes of Burkitt lymphoma?
Burkitt lymphoma starts in the B lymphocytes. As discussed above, some types of Burkitt lymphoma are associated with an Epstein-Barr virus infection or a weakened immune system. Burkitt lymphoma can also result from a chromosomal translocation involving the Myc gene. A chromosomal translocation means that the chromosome has broken. In the case of Burkitt lymphoma it affects chromosome 8 (Myc gene locus). The most common variant results in a translocation from chromosome 8 to 14 – t(8;14)(q24;q32). Many other types of Burkitt lymphoma do not have a clear cause.
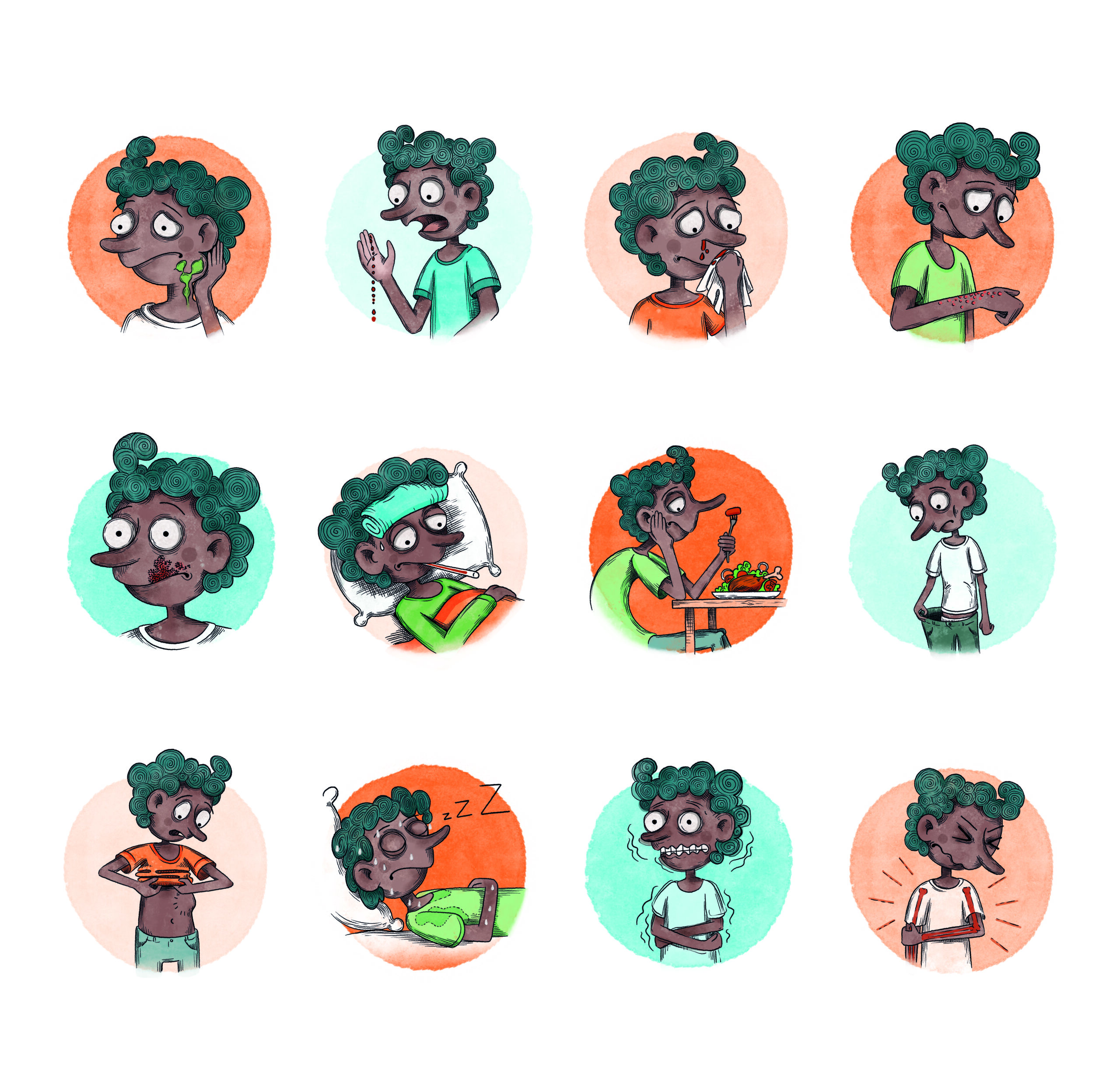
What are the symptoms of Burkitt lymphoma?
Depending on the type of Burkitt lymphoma, the patient may experience:
– Inflamed lymph nodes in the head and neck. This inflammation is often painless, but it grows very quickly.
– In terms of the sporadic variant, it starts in the abdomen and belly area, with severe pain, vomiting and nausea.
These are the two most common areas, but it can also start in other areas of the digestive system including the pancreas and liver, excretory system such as the kidneys, reproductive system such as the testicles and ovaries, as well as in the brain or cerebrospinal fluid.
Other common lymphoma symptoms also tend to be present, such as:
– Fever
– Night sweats
– Fast, obvious weight loss
– Fatigue
How is Burkitt lymphoma diagnosed?
One of the problems with Burkitt lymphoma is that, depending on the area affected, it can be difficult to differentiate the disease from others that cause, for example, intestinal occlusion and stomach pains.
It is also important to differentiate it from other tumours and lymphomas, which is why different diagnostic tests should be used:
– CT scans of the abdomen, chest and pelvis.
– Bone marrow and lymph node biopsy.
– Cerebrospinal fluid analysis.
– Complete blood counts including lactate dehydrogenase (LDH), a catalytic enzyme found in many body tissues, but with highest presence in the heart, liver, kidneys, muscles, red blood cells, brain and lungs. An abnormally high level may indicate lymphoma.
What is the treatment for Burkitt lymphoma?
If left untreated, Burkitt lymphoma becomes fatal very quickly. In fact, it is one of the fastest spreading cancers. This is why haematologists quickly start intensive chemotherapy treatment that also includes intrathecal chemotherapy (the administration of antineoplastic drugs directly into the cerebrospinal fluid). Chemotherapy may be accompanied by other treatments such as radiotherapy, steroids and other drugs.
In some rare cases of sporadic lymphoma, surgery is required in order to remove obstructed or perforated bowel segments.
What are the chances of children and teenagers with Burkitt lymphoma being cured?
The current treatment, if employed after early diagnosis, can achieve a cure in more than 80% of cases.
Links of interest concerning medical issues relating to Burkitt lymphoma in children and teenagers
About Childhood Burkitt Lymphoma. Dana Farber Cancer Institute
Types of Non-Hodgkin Lymphoma in Children. American Cancer Society
Childhood Non-Hodgkin Lymphoma Treatment. National Cancer Institute
Lymphoma in Children. St Jude Children’s Research Hospital
Useful links: local entities (resources and services)
All these organisations are external to the Josep Carreras Foundation.
ANDALUCÍA
ARAGÓN
ASTURIAS
CASTILLA LA MANCHA
CASTILLA LEÓN
CATALUÑA
VALENCIAN COMMUNITY
EXTREMADURA
GALICIA
BALEARIC ISLANDS
CANARY ISLANDS
LA RIOJA
MADRID
- AAA (asociación de adolescentes y Adultos Jóvenes con Cáncer)
- ASION
- FUNDACIÓN CAICO
- FUNDACIÓN ALADINA
- FUNDACIÓN UNOENTRECIENMIL
MURCIA
NAVARRA
BASQUE COUNTRY
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


