- OneChain Immunotherapeutics announces the treatment of the first patient in the CARxALL clinical trial evaluating its most advanced product, OC-1. The trial, conducted in Barcelona at Hospital Clínic and Hospital Sant Joan de Déu, is open to both pediatric and adult patients worldwide.
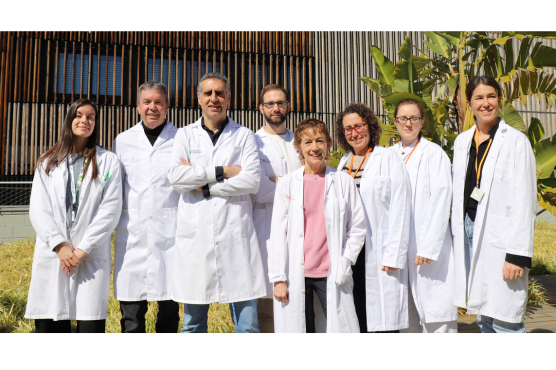
- OneChain Immunotherapeutics is a spin-off of the Josep Carreras Leukaemia Research Institute and ICREA, in partnership with Invivo Ventures, CDTI-Innvierte and the Josep Carreras Leukaemia Foundation.
- Cortical T-cell acute lymphoblastic leukemia accounts for 20-30% of T-cell leukemias and has a poor prognosis in patients who do not respond to standard treatments.
- OC -1 is a CAR-T cell therapy targeting antigen CD1a, a protein almost exclusively present on tumor cells, potentially reducing severe immunosuppression risks associated with competing CAR T treatments. It has received orphan drug designation by both EMA and the FDA.
OneChain Immunotherapeutics (OCI), a biotechnology company specializing in the development of CAR-T cell therapies for oncological diseases, announced today the first patient dosed in the CARxALL clinical trial, a study evaluating its most advanced product, OC-1, in patients with cortical T-cell acute lymphoblastic leukemia (coT-ALL). The trial, open to pediatric and adult patients worldwide, is being conducted in Barcelona at Hospital Clínic and Hospital Sant Joan de Déu, under the direction of Dr Núria Martínez and Dr Susana Rives, principal investigators for the study.
The CARxALL study (ClinicalTrials.gov identifier NCT05679895), is a dose-escalation trial, aiming to evaluate for the first time in humans the safety and tolerability of a CAR-T therapy (OC-1) in patients with coT-ALL, a subtype of leukemia that accounts for 20% of T-cell leukemias and is characterized by a poor prognosis in those patients who do not respond to existing therapies. The first patient treated at Hospital Clínic, a young man who had previously undergone several treatment lines without success, has received the full dose with no major issue.
«This treatment offers hope for patients who have exhausted all available options», explains Núria Martínez, Principal Investigator at Hospital Clínic. «It is essential that we do everything we can to ensure that as many patients as possible can access these innovative therapies. We are very grateful to OneChain for all their support with the clinical trial and hope to stablish a long-lasting relation with them. Their pipeline has a lot to offer to patients and families».
CAR-T therapies are a type of immunotherapy that involves the genetic modification of immune cells called T-cells in the laboratory, to enhance and target their ability to recognize and attack cancer cells. This strategy has already shown promising results in other forms of leukemia and lymphoma. However, applying these therapies to T-cell leukemias such as coT-ALL presents significant challenges because tumor and healthy T cells exhibit almost the same molecules on their surface. As a result, competing CAR T therapies aimed at T-ALL destroy both type of cells, potentially leading to severe immunosuppression in patients.
OC-1, the product being evaluated in the trial, aims to overcome these obstacles by targeting CD1a, a specific protein found almost exclusively in the tumor cells of patients with coT-ALL. «Our laboratory was the first to develop and validate a CAR-T specific to this therapeutic target», says Dr. Pablo Menéndez, founder of OCI and director of the stem cell biology, developmental leukemia, and immunotherapy group at the Josep Carreras Leukemia Research Institute (IJC). «Seeing now how academic work reaches patients is a dream come true for all of us».
«This is an important milestone and a very proud moment for OneChain and all our partners», said Dr. Stefanos Theoharis, CEO of the company. «Their unending support and commitment to our company and the patients has finally come to bear fruit. My heartfelt thanks go to all those individuals and organizations who have helped us achieve this milestone, including the joint effort of the Josep Carreras Leukemia Research Institute, the OneChain team, the staff at Hospital Clínic and Hospital Sant Joan de Déu, the Josep Carreras Foundation, our main investor, Invivo Partners, the Unoentrecienmil Foundation, the Banc de Sang I Teixits (BST), and the CDTI Innvierte program».