Primary immunodeficiencies
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.

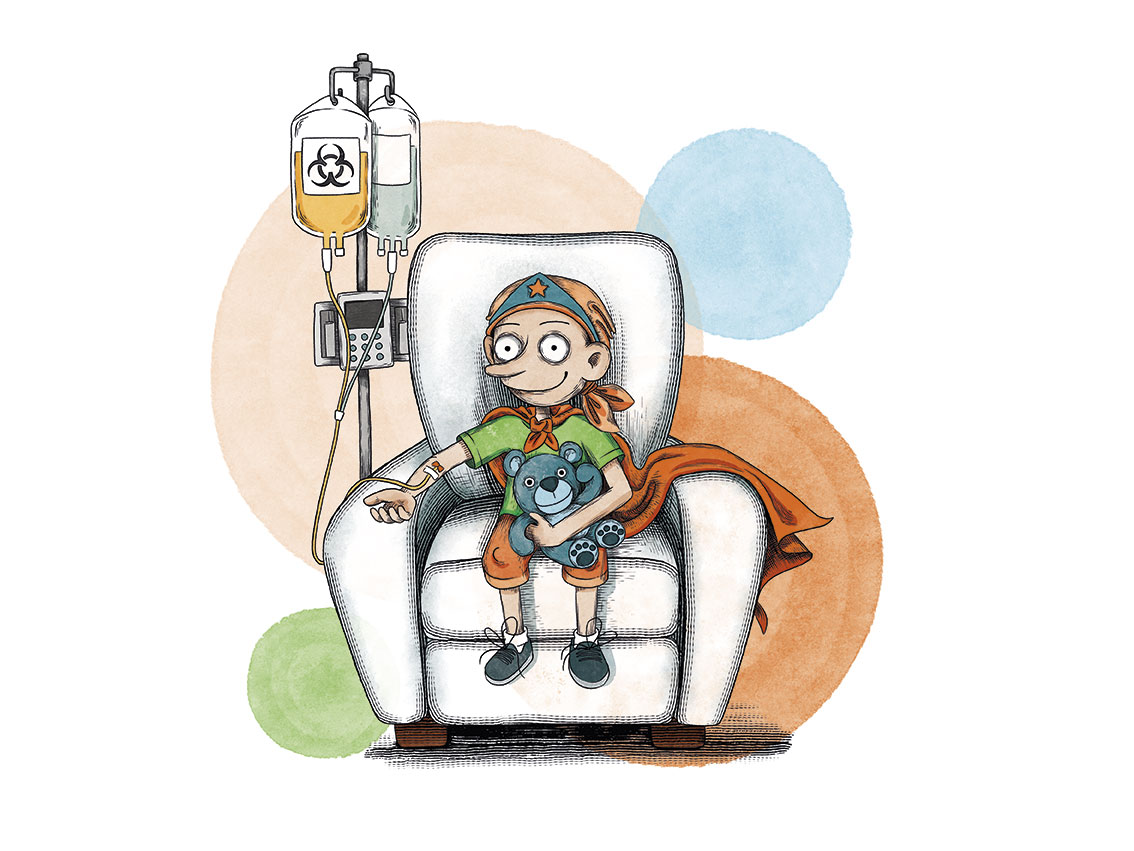
Cassià
Severe Combined Immunodeficiency.
“This is me now. My name is Cassià and I have been Unstoppable against Severe Combined Immunodeficiency since I was a baby. When I was only 6 months old, I was admitted to the hospital thinking I had meningitis, but the supposed meningitis, ended up in a completely different diagnosis. For me, a bone marrow transplant from a compatible donor was the only way to be cured, and the Josep Carreras Foundation found me that long awaited second chance. As you can see, I am doing great, studying, and passing my annual check-ups. I also play the drums, sing, participate in a group of drummers… I take advantage of any occasion to do whatever makes me happy”.
Information endorsed by… ![]()
Dr. Pere Soler Palacín. Department Head of the Paediatric Immunodeficiencies and Infectious Diseases Unit at the Vall d’Hebron University Hospital, Barcelona. (Barcelona Medical Association. Member No. 34660)
Dr. Andrea Martín Nalda. Attending physician at the Paediatric Immunodeficiencies and Infectious Diseases Unit at the Vall d’Hebron University Hospital, Barcelona. (Barcelona Medical Association. Member No. 37904)
Dr. Jacques Rivière. Attending physician at the Paediatric Immunodeficiencies and Infectious Diseases Unit at the Vall d’Hebron University Hospital, Barcelona. (Barcelona Medical Association. Member No. 49219)
Information provided by Barcelona PID Foundation
What is primary immunodeficiency (PID)?
 Primary immunodeficiencies (PID) are a group of diseases caused by quantitative and/or functional impairment of different mechanisms involved in the immune response. The differences in their clinical-immunological manifestations, especially the type of infections they present, are in each case related to molecular alterations.
Primary immunodeficiencies (PID) are a group of diseases caused by quantitative and/or functional impairment of different mechanisms involved in the immune response. The differences in their clinical-immunological manifestations, especially the type of infections they present, are in each case related to molecular alterations.
PID patients are susceptible to infections of varying severity, which, if not adequately treated, can be fatal or leave sequelae that worsen these patients’ quality of life. Moreover, an increasing examples of these diseases are appearing every day in which there is a selective susceptibility to certain microorganisms, which leads us to be more and more alert to the existence of these entities.
It is very important to keep in mind that primary immunodeficiencies are frequently associated with autoimmunity and neoplasms (especially of lymphoid tissue), with a much higher frequency than in the general population.
Primary immunodeficiencies occur in more than 1/2,000 live newborns with considerable variability between the different entities. Thus, while selective IgA deficiency is very common, affecting 1/500 people (Caucasian population), the group of severe combined immunodeficiencies (SCID) occur in about 1/50,000 live newborns.
However, it is assumed that this is a largely under-diagnosed pathology group (some reviews indicate that only 10% of existing PIDs are diagnosed). It is estimated that primary immunodeficiencies, although classified as minority diseases individually, are collectively more common than well-known diseases such as cystic fibrosis and very close to the frequency of multiple sclerosis.
Despite this, there is a great lack of knowledge about them both in the general population and in the health community.
Within primary immunodeficiencies, predominantly antibody deficiencies account for more than half of the cases, with the next most frequent group being combined T-cell and B-cell immunodeficiencies.
How are primary immunodeficiencies classified?
More than 350 primary immunodeficiencies have now been described, of which the genetic defect is known in more than 250.
The current classification was made by an international committee of experts, International Union of Immunology Societies (IUIS), which at its last biennial meeting (2017) grouped PIDs into the following 9 groups:
- Combined T-cell and B-cell immunodeficiencies
- Predominantly antibody deficiencies
- Other well-defined immune deficiency syndromes
- Diseases of immune dysregulation
- Defects in phagocyte number and/or function
- Defects in innate immunity
- Complement deficiencies
- Autoinflammatory disorders
- PID Phenocopies
What are the symptoms of primary immunodeficiencies?
With regard to the clinical suspicion index required to initiate the search for a primary immunodeficiency, there are warning signs that can guide us (modified from the warning signs proposed by the Jeffrey Modell Foundation).
- ≥ 8 acute otitis media in one year.
- ≥ 2 pneumonias (radiologically confirmed) in one year.
- ≥ 2 sinusitis in one year.
- ≥ 2 meningitis or other serious infections.
- ≥ 2 deep tissue infections in one year or of unusual location.
- Recurrent deep cutaneous infections or visceral abscesses.
- Frequent need for intravenous antibiotics to treat infections.
- Infections by unusual or opportunistic organisms.
- Family history of immunodeficiency or recurrent infections.
- Common autoimmune phenomena.
- Thrush (oral candidiasis) or cutaneous candidiasis in patients older than one year.
- Dysmorphic features associated with frequent infections.
- Post-vaccination infections in live virus vaccines.
- Delay of more than 4 weeks in the separation of the umbilical cord.
- IgE > 2000 UI/L without other apparent cause (especially with severe or recurrent skin or respiratory infections).
- Fever with suspected periodicity.
- Bronchiectasis without apparent cause.
 However, it is important to keep in mind that it is usually the sum of two or more of these signs and symptoms that leads to a real suspicion of primary immunodeficiency. In addition, the weight of each of the variables is different and is particularly important for the following variables: recurrent pneumonia, severe or opportunistic infections and family history of primary immunodeficiency.
However, it is important to keep in mind that it is usually the sum of two or more of these signs and symptoms that leads to a real suspicion of primary immunodeficiency. In addition, the weight of each of the variables is different and is particularly important for the following variables: recurrent pneumonia, severe or opportunistic infections and family history of primary immunodeficiency.
These warning signs exist for both children and adults (with some modifications).
How is a primary immunodeficiency diagnosed?
In recent years, Catalonia has led a project to use these warning signs (revised in the form of a computer algorithm) to guide primary care professionals in the early detection of possible primary immunodeficiencies. This project called PIDCAP has been active since 2017 in the city of Barcelona with promising results.
Although it is not yet available for the entire Spanish health system, there is a common early diagnosis technique for the different genetic forms of severe combined immunodeficiency (SCID) applicable in the newborn dried blood heel prick test called T-cell Receptor Excision Circles (TRECs).
This initiative has recently emerged as a useful non-invasive tool to investigate T-lymphocyte production by the thymus. The data provided in the different US states where it has been applied since 2008 demonstrate its usefulness in the diagnosis and treatment of these patients, with a very low percentage of false positives and negatives and a clear improvement in the vital prognosis of these patients. In Catalonia, universal screening of all newborns has been carried out since January 2017 and it has already enabled the detection and treatment of severe immunodeficiencies.
At what age do the clinical manifestations of a primary immunodeficiency begin?
 Although most primary immunodeficiencies present in childhood, they can manifest at any age and it is very important to also think of these entities in the adult patient. The age of onset of symptoms can also be used as a guide to one immune system defect or another.
Although most primary immunodeficiencies present in childhood, they can manifest at any age and it is very important to also think of these entities in the adult patient. The age of onset of symptoms can also be used as a guide to one immune system defect or another.
By way of example, severe infections during the first months of life are indicative of primary combined immunodeficiency, however in predominantly humoral primary immunodeficiencies, infections usually begin after 5-6 months of life, at which time maternal immunoglobulins are no longer present.
Common variable immunodeficiency can present at any age, although as with IgA deficiency, the diagnosis cannot be confirmed until the patient has reached the age of 4 years. However, it should be kept in mind that these are only indicative data, as more and more “atypical” forms of certain PIDs are described that present milder and later than the classic forms.
How is a primary immunodeficiency diagnosed (laboratory studies approach)?
It should be borne in mind that the vast majority of primary immunodeficiencies are diagnosed with a correct clinical history and physical examination, a complete blood count and plasma immunoglobulin (Ig), and these tests are available in most laboratories and in primary care.
Thus, in case of suspected primary immunodeficiency, the initial study should include:
- Blood count, with differential blood cell count, where we can recognise lymphopaenia or neutropaenia.
- Serum Ig counts (IgG, IgM and IgA): to mainly assess hypogammaglobulinaemia. We must also consider special situations of differential diagnosis or targeted suspicion where an IgE can be very useful.
A second diagnostic step would include:
- The determination of functional antibodies against protein antigens, such as tetanus, or polysaccharides such as pneumococcus or Salmonella typhi. These may be absent even if we previously had total Ig levels in the normal range.
- Lymphocyte immunophenotype: CD3+ (T lymphocytes), CD3+CD4+, CD3+CD8+, CD4/CD8 ratio, CD19 (B lymphocytes) and CD56+ (NK).
- Proliferative function of lymphocytes. Assesses the ability of the lymphocytes to react in vitro to different stimuli in order to draw parallels to what might occur in vivo. It is used to detect cases of combined immunodeficiency.
- In case of leukocytosis with normal or high Ig, and the presence of abscesses in the skin or different organs, a test of the oxidative capacity of granulocytes by flow cytometry (to rule out chronic granulomatous disease) and assess for leukocyte adhesion deficit (although this is an extremely rare entity).
- Complement study with CH50 and AP50.
- Genetic studies (Sanger, IDP panels, exome, genome, array-CGH, etc.)
It is important to assess the results according to the reference values for each age, as there are significant differences which, if not taken into account, may lead to overlooking the diagnostic suspicion of primary immunodeficiency.
Guidance is always important, depending on the diagnostic suspicion, to avoid unnecessary tests that waste time and resources. However, when the diagnosis is uncertain and suspicion is high, additional tests such as functional or molecular studies are necessary and should be performed at reference centres.
What is the treatment for primary immunodeficiencies?

Leo
Severe Combined Immunodeficiency.
“Hi, I’m Silvia, the mom of Leo, the submarine captain. In 2022 we celebrate his 10th birthday! When he was just a baby, Leo underwent a bone marrow transplant from an anonymous donor that saved his life. Leo was diagnosed as a baby with severe combined immunodeficiency, a severe and rare disease, what they call a ‘bubble boy’. As a result, the little boy’s body cannot fight infections and life in a normal environment can be fatal. It is the most severe of the primary immunodeficiencies, and his only chance of survival is a bone marrow transplant. He was admitted to the hospital when he was just 8 months old and was able to leave when he was about to turn 18 months old, so he spent 10 months in his ‘submarine’, my little Captain Unstoppable. I want to remind you that there is no greater pride than to be able to give someone a second chance, this gesture not only gives life, but should make us infinitely happy”.
Advances in knowledge regarding aetiology, clinical and therapeutic aspects have profoundly improved the prognosis of these patients in recent years. The treatment of patients with primary immunodeficiency is divided into the so-called support treatment and curative treatments as described below.
Support treatment
- Immunoglobulin (Igs) replacement therapy:
Igs are plasma preparations drawn from a pool of thousands of donors. They contain neutralising antibodies against numerous viral and bacterial pathogens. They undergo sterilisation processes that eliminate other proteins and live viruses such as HBV, HIV, HCV. It is the treatment of choice for patients with significant alterations in humoral immunity such as common variable immunodeficiency (CVID), X-linked agammaglobulinemia (XLA), and antibody production defects, as well as combined immunodeficiencies and many other immunodeficiency-associated syndromes. They can be administered intravenously or subcutaneously and reduce the incidence and severity of infections, thereby reducing morbidity and mortality in these patients.This requires maintaining serum IgG trough concentrations above 600-800 mg/dl before further administration, although both the dose and the trough concentrations to be obtained must be individualised for each patient according to their infection rate. - Antimicrobial treatment:
Antimicrobial therapy should be initiated early in patients with infectious manifestations. Adequate cultures are essential because of the possibility of opportunistic pathogens that are common in patients with primary immunodeficiencies. Prophylactic antibiotics, not routinely recommended, are sometimes indicated to protect the patient from pathogens to which he or she may be susceptible. An example of this is the treatment with trimethoprim-sulfamethoxazole in patients with hyper IgM syndrome and in those with T-cell defects following haematopoietic precursor transplantation for protection against Pneumocystis jirovecii pneumonia.Primary antimicrobial prophylaxis is essential in phagocytic defects and should be considered for complement defects and in hyper IgE syndrome. In certain PIDs with a high susceptibility to bacterial, fungal or viral infections, prolonged antimicrobial prophylaxis is necessary and should be assessed on an individual basis.
- Other therapies:
Enzyme replacement has been used in ADA deficiency, the first human enzyme deficiency to be treated with replacement therapy.In addition, interferon gamma has been used as a treatment in chronic granulomatous disease and immunisations against encapsulated microorganisms are recommended in certain complement deficiencies. Plasma concentrate derivative of recombinant C1 esterase inhibitor is available for the treatment of hereditary angioedema. Similarly, certain immunodeficiencies with autoimmune or inflammatory complications require immunosuppressive treatments such as mycophenolate, rapamycin, ruxolitinib and other monoclonal agents.
Curative treatments
- Haematopoietic precursor transplantation (bone marrow transplantation):
Haematopoietic precursor transplantation (bone marrow transplantation) is, together with gene therapy, the only curative option for many primary immunodeficiencies. It is the treatment of choice for some immunodeficiencies such as severe combined immunodeficiency (SCID), Wiskott-Aldrich syndrome, chronic granulomatous disease, among others.
In patients with severe combined immunodeficiency (SCID) who receive a transplant from an HLA-identical donor, survival rates reach 90%; this is similar to when the transplant is from a non-familial but matched donor and performed very early. Early diagnosis and the search for optimal donors, together with conditioning, where appropriate, achieves more favourable outcomes.
Gene therapy:
Gene therapy is becoming a reality for many primary immunodeficiencies such as Wiskott-Aldrich syndrome, ADA deficiency, some forms of SCID, some forms of chronic granulomatous disease and others. Although several PIDs have been successfully treated in early trials, the outcome of this therapy is mixed and, unfortunately, several patients have subsequently developed myelodysplastic syndrome associated with the activation of proto-oncogenes by the vector. With the use of new vectors in the last decade, multiple successful gene therapies have been performed without these undesirable effects and are now a viable option for a variety of PIDs.
What are the chances of children with a severe combined immunodeficiency being cured?
Without treatment, severe combined immunodeficiency often leads to severe infection and death in children by the age of two. If performed within the first few months of life and from an HLA-identical sibling, the bone marrow transplantation can allow for a long-term survival rate of more than 90%.
Links of interest concerning medical issues relating to primary immunodeficiencies
Information on severe combined immunodeficiency. National Center for Advancing Translational Sciences
We recommend visiting the following websites of specialised foundations:
If you have PID or you are a family member, you can also access the different family associations in Spain:
www.abadip.org
Links of interest on other topics related to primary immunodeficiencies
All these organisations are external to the Josep Carreras Leukaemia Foundation.
ANDALUCÍA
ARAGÓN
ASTURIAS
CASTILLA LA MANCHA
CASTILLA LEÓN
CATALUÑA
VALENCIAN COMMUNITY
EXTREMADURA
GALICIA
BALEARIC ISLANDS
CANARY ISLANDS
LA RIOJA
MADRID
- AAA (asociación de adolescentes y Adultos Jóvenes con Cáncer)
- ASION
- FUNDACIÓN CAICO
- FUNDACIÓN ALADINA
- FUNDACIÓN UNOENTRECIENMIL
MURCIA
NAVARRA
BASQUE COUNTRY
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


