Chronic myelomonocytic leukaemia
Until a few years ago, chronic myelomonocytic leukaemia was classified as a type of myelodysplastic syndrome. The fact that, in addition to dysplasia, there is an excess of monocytes has led to a separate classification as a myelodysplastic/myeloproliferative neoplasm.
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.

Angel
Chronic myelomonocytic leukemia.
“In 2020 I underwent a bone marrow transplant from an anonymous donor located by the REDMO program of the Josep Carreras Foundation. A year earlier I was diagnosed with chronic myelomonocytic leukaemia. But between the fantastic team at the hospital and the Josep Carreras Foundation, a miracle was wrought. It was not easy. I am from Zaragoza and they transferred me to Barcelona. After a month and a half in the hospital, I was in an apartment for patients during three months near Barcelona. The recovery went well, little by little, I was feeling better. I have never felt better cared for! There is not a day that I do not remember my donor, the team of doctors who took care of me and, above all, the Josep Carreras Foundation.”
Information endorsed by… ![]()
Information provided by Dr. Enric Carreras Pons. Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Haematology and Haemotherapy and Medical Director of the Josep Carreras Foundation. Barcelona Medical Association (Co. 9438).
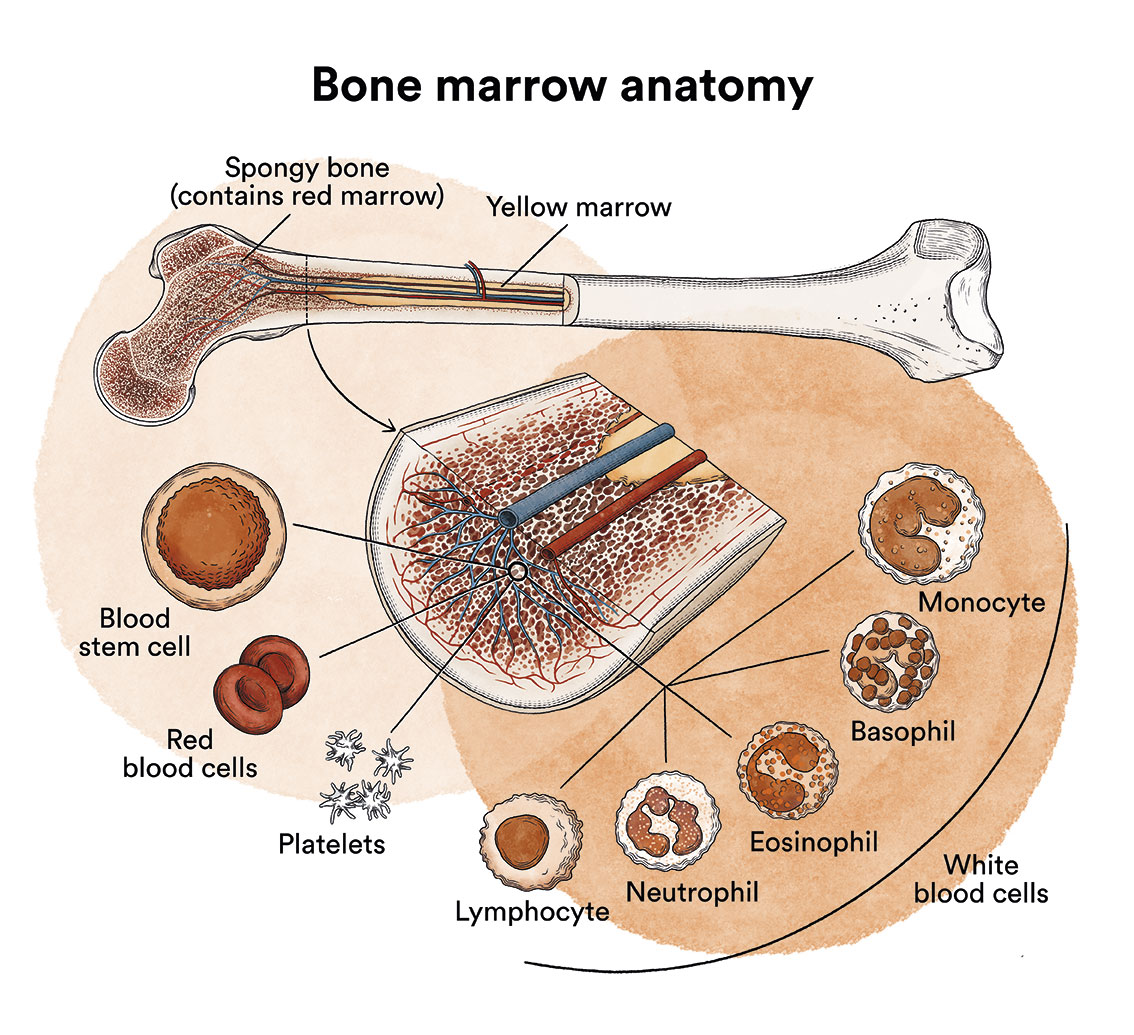
How does bone marrow work and what are the types of blood cells?
Chronic myelomonocytic leukaemia (CMML) is a type of blood cell and bone marrow cancer. See section Leukaemia, bone marrow and blood cells.
What is chronic myelomonocytic leukaemia and who does it affect?
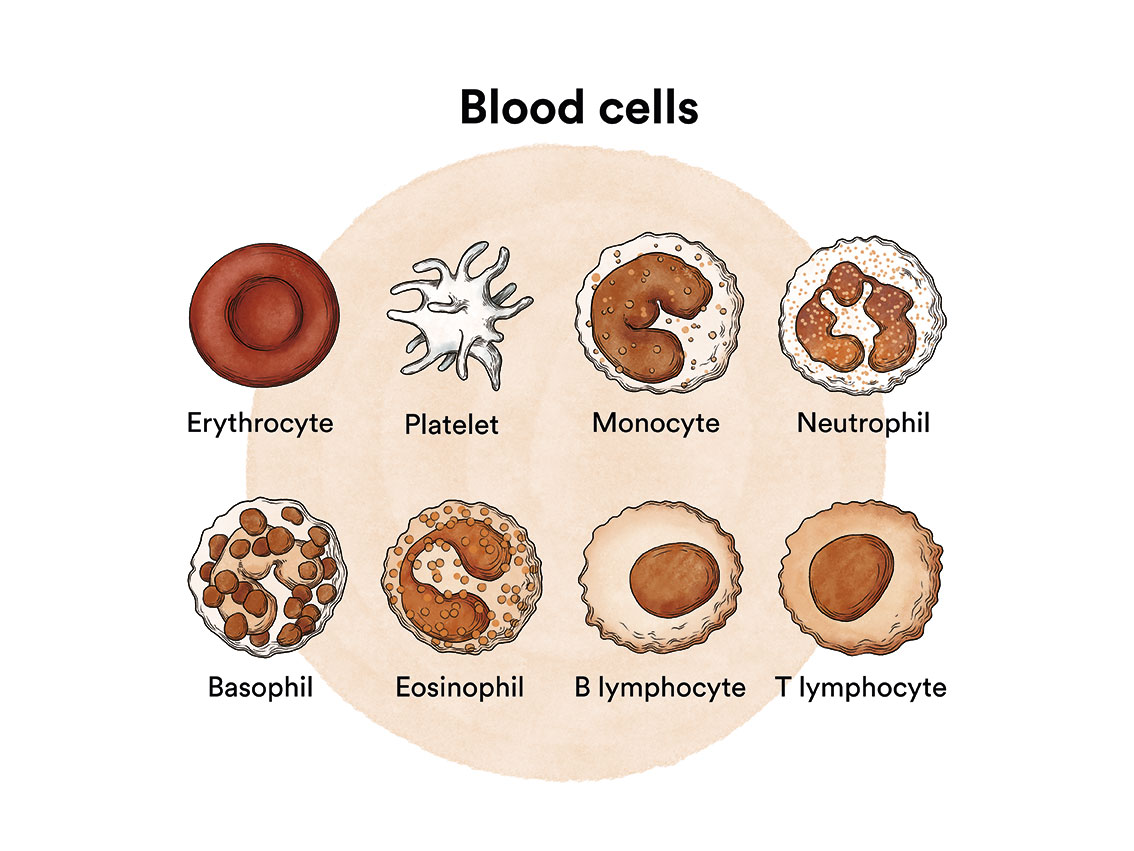
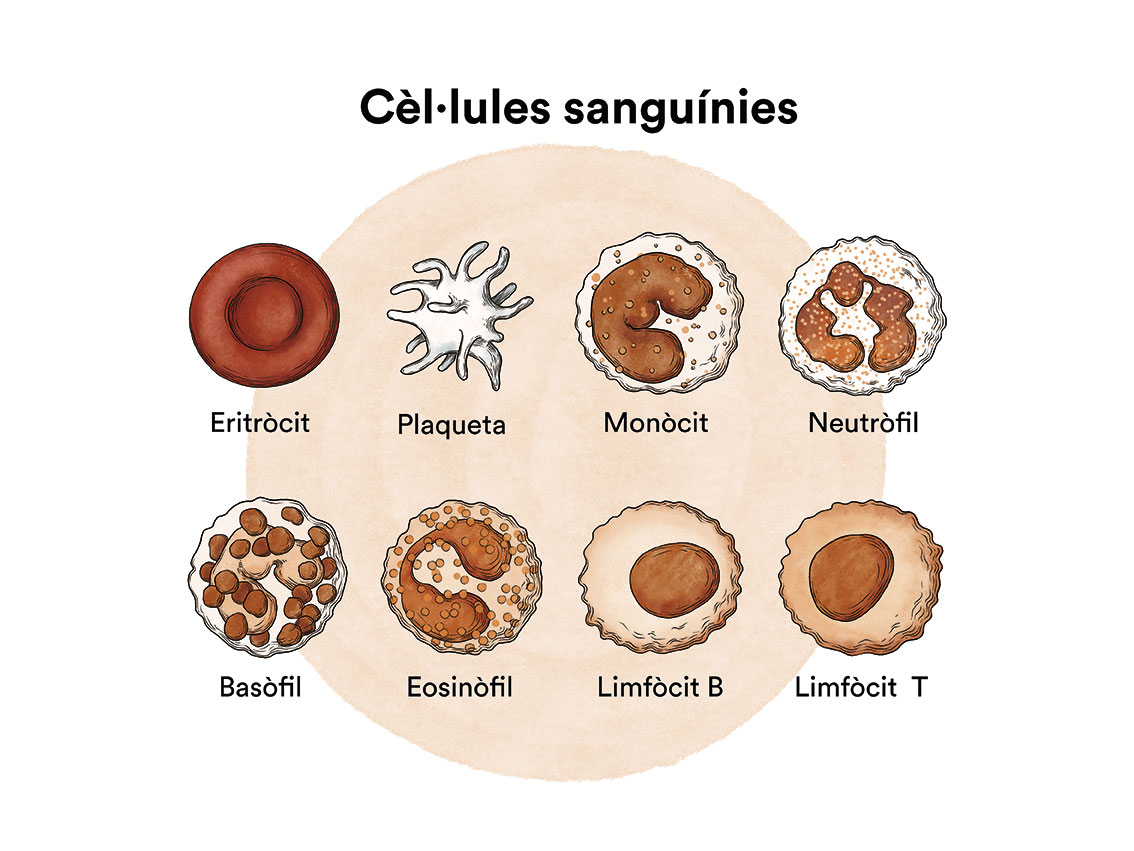
Chronic myelomonocytic leukaemia (CMML) is a type of disease of the bone marrow, the organ responsible for making blood cells (red blood cells, white blood cells and platelets). Under normal conditions, these cells reproduce and mature in the bone marrow until they emerge and circulate in the blood. In chronic myelomonocytic leukaemia, the bone marrow produces these cells abnormally, both in number and in maturation or function, and these abnormalities are detected in the blood when we run a blood test (haemogram) and look at the blood under a microscope.
In CMML, the cell that does not function as it should and increases uncontrollably are monocytes, a type of white blood cell. Monocytes, along with other white blood cells called neutrophils, are the two main cells that ingest and kill microbes in the blood. When monocytes leave the blood and enter the tissue, they become macrophages. Macrophages are monocytes in action: they can fight infections in tissues, ingest dead cells and help other cells, such as lymphocytes, carry out their immune functions.
Like all blood cells, monocytes originate from immature blood-producing cells called “stem cells”. In CMML, too many stem cells have transformed into monocytes. Over time, monocytes accumulate in the bone marrow and other organs and interfere with the normal production of other types of blood cells, including red blood cells (which carry oxygen to all tissues in the body) and platelets (which form clots to help stop bleeding from injury).
Chronic myelomonocytic leukaemia mainly affects people over 60 years of age at diagnosis.
It is important to differentiate between chronic myelomonocytic leukaemia and chronic myeloid leukaemia which, despite their similar names, are completely different entities.
How is chronic myelomonocytic leukaemia classified?
Chronic myelomonocytic leukaemia (CMML) is classified into several subtypes based on the number of immature cells (blasts) in the bone marrow:
Type 0: there are less than 5% blasts in the bone marrow and less than 2% in the blood.
Type 1: there are 5-9% blasts in the bone marrow and 2-4% in the blood.
Type 2: there are 10-19% blasts in the bone marrow and 5-19% in the blood.
What are the causes of chronic myelomonocytic leukaemia?
It is not known why chronic myelomonocytic leukaemia occurs, but in most cases, it is an acquired disease related to ageing or due to environmental exposure, occupational or otherwise, to toxic substances or treatments such as radiotherapy and/or chemotherapy, among others.
Chronic myelomonocytic leukaemia, like other cancers, is not contagious. See section Leukaemia, bone marrow and blood cells.
What are the symptoms of chronic myelomonocytic leukaemia?
In the early stages of chronic myelomonocytic leukaemia, patients often do not feel any discomfort. In these cases, the diagnosis is usually discovered after results indicating low blood cell counts in a control blood test or for other medical procedures.
In cases in which the patient feels unwell and visits their doctor, the symptoms and severity will depend on the type of cells affected and on how low the blood cell counts are.
If there is anaemia due to a decrease in red blood cells , tiredness and weakness are common (when it is severe, the patient may also experience dizziness, palpitations, sweating…). In more severe cases there may be symptoms resulting from decreased white blood cells and/or platelets leading to infections and/or haemorrhages, respectively.
There may be petechiae (pinhead-sized red spots on the skin), bruising and bleeding due to thrombocytopaenia (insufficient platelets).
In addition, as the bone marrow works at a faster rate than normal, the liver and spleen may increase in size so that they also contribute to this proliferation; this increase in size can lead to abdominal discomfort (bloating, pain, constipation…).
There may also be symptoms such as tiredness, lack of appetite, weight loss, itching (these are known as constitutional symptoms).
How is chronic myelomonocytic leukaemia diagnosed?
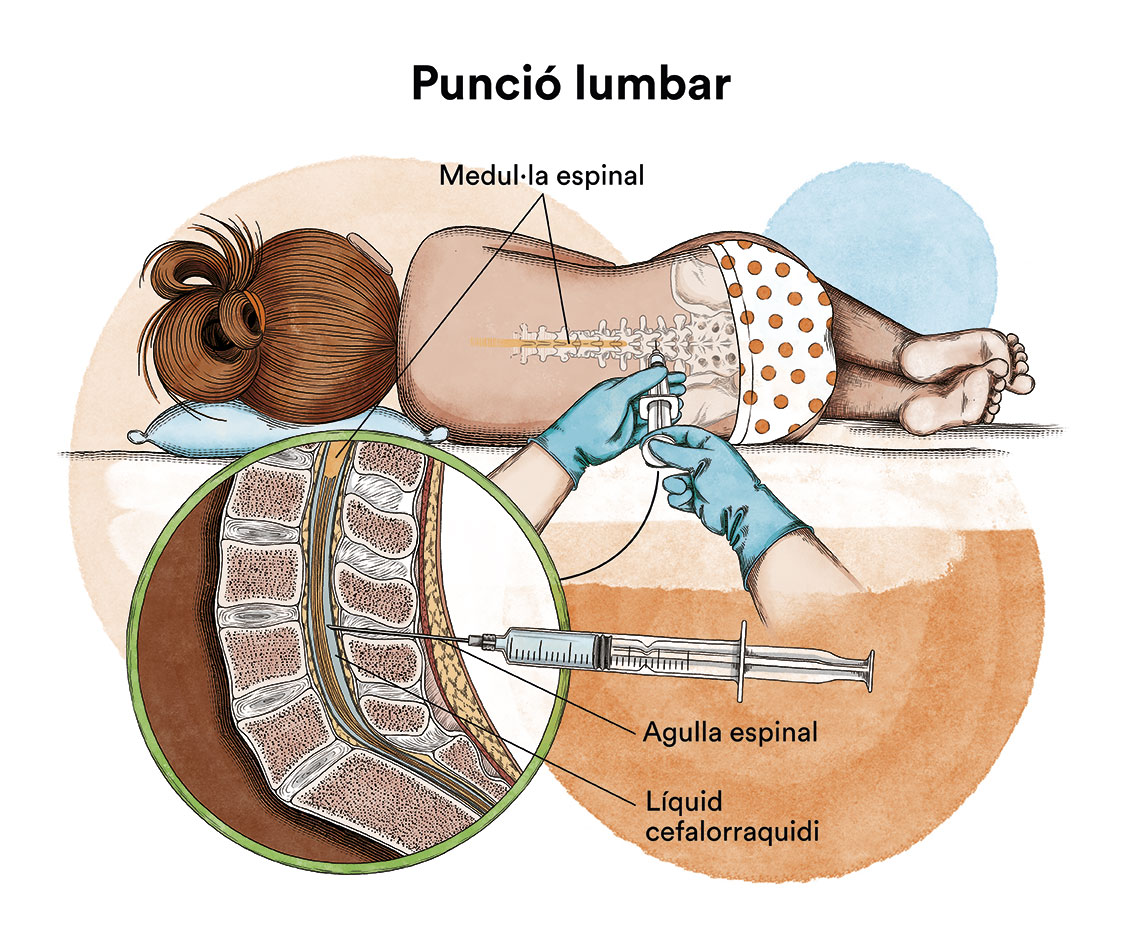
It is not normally possible to confirm the diagnosis of chronic myelomonocytic leukaemia (CMML) with a blood test alone. To confirm the diagnosis, the patient should be monitored for a period of time, laboratory tests repeated and the results evaluated to rule out other myelodysplastic syndromes and myeloproliferative neoplasms. The results of a blood smear and bone marrow aspiration and biopsy need to be analysed in order to diagnose chronic myelomonocytic leukaemia.
In these analyses, the results show:
– Persistent high level of monocytes in the blood (more than 1,000 monocytes per microlitre of blood [1,000/µl])
– No evidence of the Philadelphia chromosome (which is seen in chronic myeloid leukaemia, a different entity as discussed above)
– Increased eosinophils (a type of white blood cell); if the eosinophil count is elevated, it is also recommended that the patient be tested for genetic changes related to platelet growth factors
– Less than 20% blasts in blood and bone marrow; blasts include myeloblasts, monoblasts and promonocytes (types of immature white blood cells)
– Abnormal changes in one or more types of the precursor cells that develop into red blood cells, certain white blood cells or platelets; these abnormalities are known as ‘dysplasias’, involving abnormal cell growth.

In addition to basic blood and bone marrow studies (morphology, blood count, immunophenotyping), cytogenetic studies (to detect specific chromosomal abnormalities) and molecular studies (to detect specific genetic alterations) are essential for typing and classifying the disease. Certain genetic and molecular alterations correlate with treatment sensitivity and prognosis. Approximately 30% of patients with chronic myelomonocytic leukaemia have chromosomal abnormalities. Between 1% and 4% of patients with chronic myelomonocytic leukaemia have an abnormality known as ‘translocation’, where part of a chromosome breaks off and attaches to another chromosome, which can lead to the development of an oncogene (cancer-causing gene).
In CMML, the translocation sometimes includes the PDGFR-β and TEL genes. Patients with PDGFR-β and TEL gene mutations may respond favourably to treatment with the drug imatinib mesylate (Gleevec®). The most common cytogenetic abnormality in chronic myelomonocytic leukaemia is an extra copy of chromosome 8. This anomaly is associated with an unfavourable prognosis.

An internationally agreed prognostic system is used to establish the level of risk for each of the myelodysplastic syndromes and is constantly being revised. In other words, it is a system that aims to elucidate more precisely whether the disease will be more or less aggressive. This index is called the IPSS-R and is based on data from thousands of patients internationally.
This index is based on:
- the number of blasts in the bone marrow
- type of blood cells which are altered (haemoglobin and platelets)
- whether the bone marrow cells have altered chromosomes.
The Spanish Myelodysplastic Syndromes Group (GESMD) developed a prognostic scale for CMML, the CPSS, from a group of Spanish patients. It also confirmed the usefulness of the scale in an independent group of patients from international centres.
Chronic Myelomonocytic Leukaemia Prognostic System (CPSS)
.
| Variable | 0 | 1 | 2 |
| WHO diagnosis | CMML-1 | CMCL-2 | |
| Variant according to FAB | Myelodysplastic variant | Myeloproliferative variant | |
| Transfusion dependency | No | Yes | |
| Cytogenic Category | Low risk | Intermediate risk | High risk |
A person can have a CMML that is low, intermediate, or high risk. Doctors can use this increased or decreased risk to recommend the most appropriate treatment. A person with low-risk disease may survive for years with few or no symptoms and may not need any treatment. A person at intermediate or high risk may need to initiate some form of therapy. However, each person may respond differently to treatment. A person’s age, general health and other factors greatly influence the response to the disease and how well the drugs are tolerated. The physician will also take all these factors into account when recommending treatment. There are other prognostic scores that include, in addition to cytogenetics, the presence of molecular factors such as ASXL1, NRAS, SEPB1 and RUNX1, which are also key to the choice of the ideal treatment.
What is the treatment for chronic myelomonocytic leukaemia?
 There is no standard treatment for CMML. Treatment may include administration of standard or low doses of cytarabine (Cytosar-U®), etoposide (VePesid®) and hydroxyurea (Hydrea®). Treatment with these drugs has proved useful in a small number of patients. Other drugs approved for the treatment of chronic myelomonocytic leukaemia include azacitidine (Vidaza®) and decitabine (Dacogen®). These drugs, known as “hypomethylating agents”, affect the way genes are controlled. They appear to help prevent abnormal cells in the bone marrow from dividing to form new cells and increase their susceptibility to death. Long-term outcome studies have demonstrated the efficacy of these drugs in some patients with chronic myelomonocytic leukaemia.
There is no standard treatment for CMML. Treatment may include administration of standard or low doses of cytarabine (Cytosar-U®), etoposide (VePesid®) and hydroxyurea (Hydrea®). Treatment with these drugs has proved useful in a small number of patients. Other drugs approved for the treatment of chronic myelomonocytic leukaemia include azacitidine (Vidaza®) and decitabine (Dacogen®). These drugs, known as “hypomethylating agents”, affect the way genes are controlled. They appear to help prevent abnormal cells in the bone marrow from dividing to form new cells and increase their susceptibility to death. Long-term outcome studies have demonstrated the efficacy of these drugs in some patients with chronic myelomonocytic leukaemia.
The small number (about 1-4%) of patients with PDGFR-β and TEL gene mutations are treated with imatinib mesylate (Gleevec®). This treatment usually results in blood cell counts returning to normal levels, as well as cytogenetic remissions and occasionally molecular remissions in these patients with chronic myelomonocytic leukaemia.
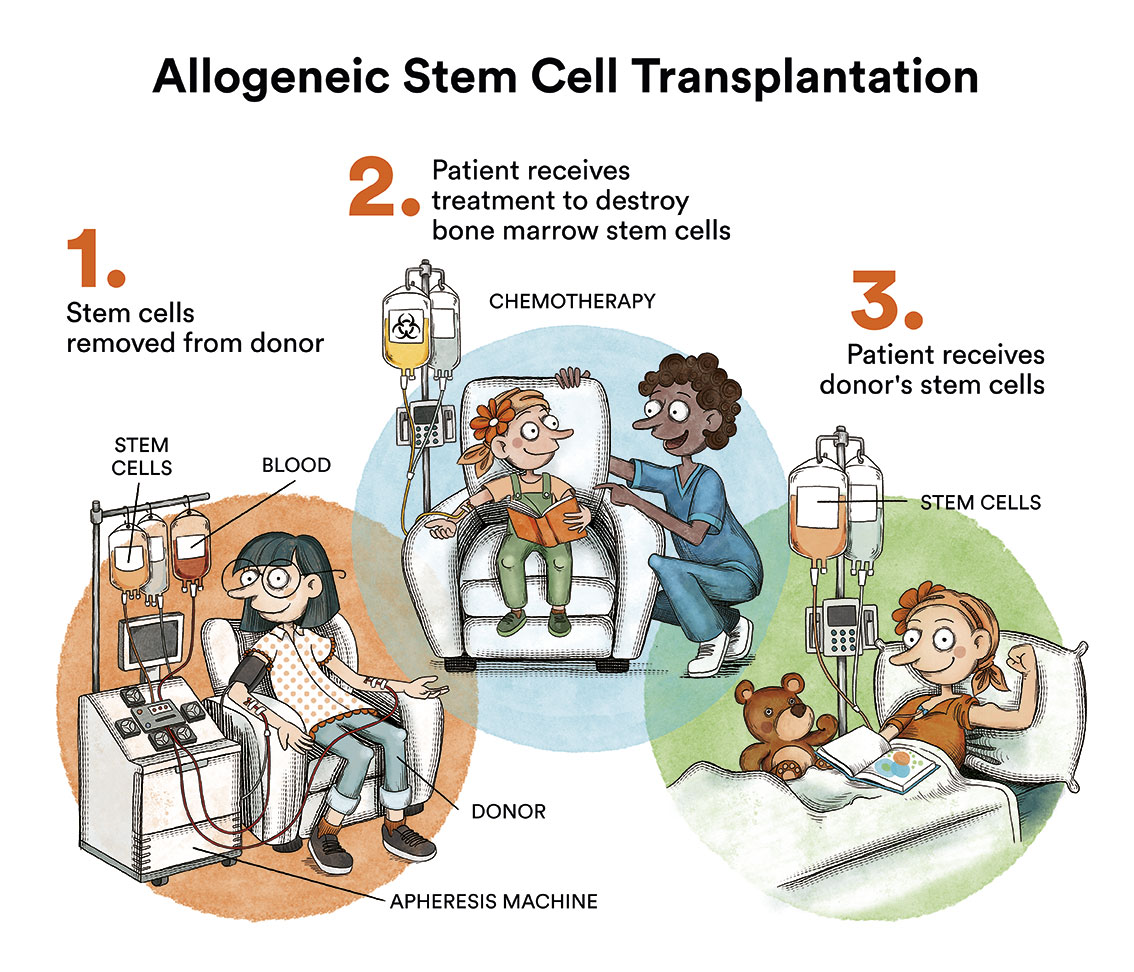
The only curative option for CMML is an allogeneic bone marrow transplantation. However, this therapy has a significant life-threatening risk and is reserved for patients under 70 years of age with a high risk of chronic myelomonocytic leukaemia transforming into acute leukaemia. In 20% of cases the leukaemia progresses to acute myeloid leukaemia
Blood transfusions (supportive therapy)
Many patients with myelodysplastic syndromes and chronic myelomonocytic leukaemia are highly dependent on blood transfusions due to the depletion of certain blood cells. These transfusions are usually performed in the day hospital on an outpatient basis. Red blood cell transfusions are common in some patients. However, sometimes it may also be necessary to receive a transfusion of platelets or white blood cell stimulating factors (G-CSF).

Side effects of blood transfusion therapy are rare, but transfusion reactions, infections, development of antibodies to red blood cells or platelets, and iron overload in different organs of the body may be observed.
New treatments: disease-modifying therapies
When a cure for chronic myelomonocytic leukaemia is not possible because the patient cannot undergo a bone marrow transplant, there are drugs that can modify the course of the disease in order to improve bone marrow function. One of these is azacitidine (Vidaza®), which is commonly used to prevent dependence on blood transfusions, to prevent bleeding and/or infections. Azacitidine belongs to a class of medicines called demethylating agents. It works by helping the bone marrow to produce normal red blood cells and destroying abnormal cells in the bone marrow. Apart from bone marrow transplantation, azacitidine is the first treatment that has proven to delay progression to acute leukaemia and prolong life in patients with MDS and CMML. Not least, it has also been shown to improve the quality of life of treated patients.
What are the chances of chronic myelomonocytic leukaemia patients being cured?
Unfortunately, long-lasting remissions are not common. The median survival time reported for people diagnosed with chronic myelomonocytic leukaemia is 12-24 months after the start of treatment.
Links of interest concerning medical issues relating to chronic myelomonocytic leukaemia
What is chronic myelomonocytic leukaemia (CMML)? Cancer Research UK
Chronic myelomonocytic leukaemia. The Leukaemia Foundation
Chronic myelomonocytic leukemia. Leukemia & Lymphoma Society
Links of interest on other topics related to chronic myelomonocytic leukaemia
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia or cancer patients:
In Spain there is a large network of associations for haematological cancer patients that, in many cases, can inform you, advise you and even carry out certain procedures. These are the contacts of some of them by Autonomous Communities:
All these organisations are external to the Josep Carreras Foundation.
STATE
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact with the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- Josep Carreras Leukaemia Foundation
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!