Adult Hodgkin’s lymphoma
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.
The lymphomas are a heterogeneous group of cancers of the blood, specifically of the lymphatic system. The lymphatic system is a network of organs (spleen and thymus), lymph nodes, lymph ducts and vessels that produce and transport lymph from the tissues to the bloodstream. It is a key part of our body’s immune system and helps protect the body against germs, including bacteria and viruses.
Traditionally, lymphomas are divided into two main groups: Hodgkin’s lymphoma, usually a single clinical entity with several stages and the non-Hodgkin’s lymphomas a heterogeneous group with more than 60 types of non-Hodgkin’s lymphomas with radically different treatments and prognoses.
Hodgkin’s lymphoma can affect children, adolescents and adults. Information on paediatric cases can be found at Haematological diseases in children .

Ana
Hodgkin lymphoma.
“When I was 26 years old I was diagnosed with Hodgkin lymphoma. Before the first chemo session I was afraid, I didn’t know how I was going to face ir, how I could continue with a smile on my face every day. But at the moment I sat down on the chair in the haematology room, with the three yellow bags of chemotherapy, I knew I had two options: stay behind with my illness or look forward, being happy and trying to look at the good side of all that. Of course, I chose the second option, and although people may not believe it, this disease does have a good side. From that day I began to be stronger, braver, and to think that I could handle this disease. I thought about making a list of things and I titled it ‘Wishes that an illness will not prevent me from fulfilling’. Today I have already fulfilled many of my wishes, among them, being a mother.”
Information endorsed by… ![]()
Information reviewed by Dr. Ana Sureda, Head of the Clinical Haematology Service of the Catalan Institute of Oncology Duran y Reynals. Barcelona Medical Association (Co. 27748)
What is adult Hodgkin’s lymphoma and who does it affect?
Hodgkin’s lymphoma is a cancerous disease of the lymph nodes. The lymphatic system is a network of organs, lymph nodes, ducts and blood vessels that produce and transport lymph from tissues to the bloodstream. It is a fundamental part of the body’s immune system (see next section).
The malignant cells responsible for the disease are the so-called Reed Sternberg cells, which are B-lymphocytes. However, if you look at the lymph node of a patient with Hodgkin’s lymphoma under the microscope you will see that Reed Sternberg cells represent only a small proportion of the cells that occupy the node (5%). The rest of the lymph node is occupied by the so-called “inflammatory infiltrate” made up basically of T-lymphocytes and other cells such as eosinophils, macrophages… Although Hodgkin’s lymphoma is a disease of the lymph nodes and these are the main organs affected, all those areas of our body containing lymphoid tissue can be affected in this disease (liver, spleen, bone marrow, tonsils…). However, this involvement is rare, at least at the time of diagnosis of the disease.
Hodgkin’s lymphoma is a rare disease. It represents approximately 20-25% of all lymphomas, has an incidence of 30 new cases per million inhabitants per year in Spain and has two peaks of incidence. The first is in young patients, between 15 and 35 years of age, and the second in older patients, from 55 years of age onwards. The first peak is more frequent in women and the second in men. According to data from the Spanish Society of Medical Oncology (SEOM), approximately 1,500 new cases of Hodgkin’s lymphoma are diagnosed in Spain each year.
The latest World Health Organization classification divides Hodgkin’s lymphoma into two main subtypes: classical Hodgkin’s lymphoma (80% of cases) and nodular lymphocyte predominant Hodgkin’s lymphoma (20% of cases), as will be described below.
Africa
Hodgkin’s lymphoma.
“When I was 23 years old I was diagnosed with Hodgkin lymphoma. I underwent 12 heavy chemo sessions and did not need radiotherapy. I was lucky to have a complete remission. How does it is? Well, very bad. At that moment you only think about finishing and you are not very aware of what you are going through. When you finish, your life is completely upside down, but you feel very lucky to be able to tell it. Nowadays I go to my check-ups where they tell me that I am doing great. I have returned to health, to feeling good. Physically I am back to what I was before. I have a job that I love and I have been a mother. Sometimes it’s hard for me to believe that after something so bad, something so good and so desired has come to me. ”
The lymphatic system
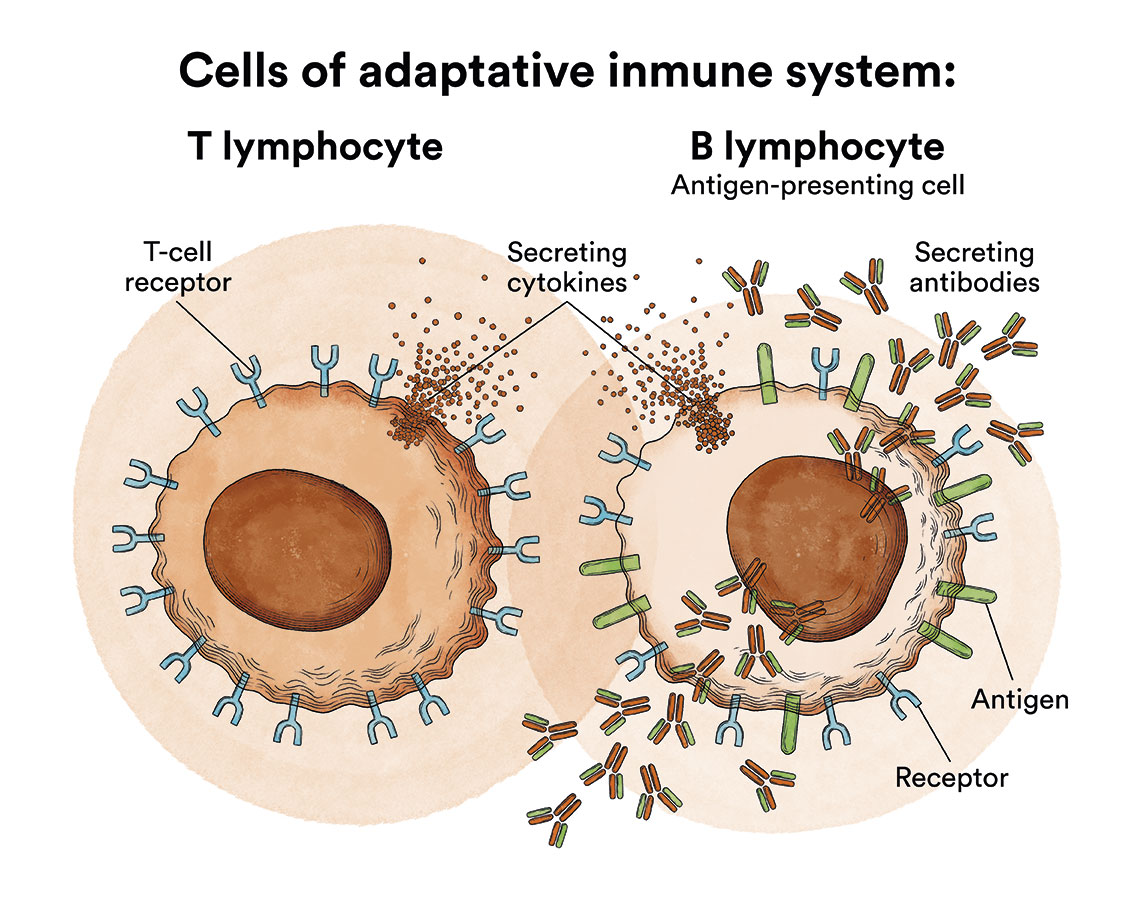
The lymphatic system is mainly made up of cells called lymphocytes, a type of white blood cell. There are two main types of lymphocytes in our blood, called B-lymphocytes (B cells) and T-lymphocytes (T cells).
- B-lymphocytes: They make up 5-15% of all lymphocytes and give rise to plasma cells that produce antibodies and help protect the body against bacteria or viruses. Antibodies attach to germs, and mark them for destruction by other components of the immune system.
- T-lymphocytes: They are responsible for coordinating the cellular immune response and are responsible for cooperation in the development of all forms of immune response, including the production of antibodies by B-lymphocytes. There are several types of T-cells, each with a special function. Some T-cells destroy germs or abnormal cells in the body. Other T-cells stimulate or slow down the activity of other immune system cells.
Circulating B and T lymphocytes are derived, like all blood cells, from haematopoietic stem cells in the bone marrow. The stem cell gives rise, among others, to lymphoblasts (more immature lymphoid cells) and from these, after successive maturation stages, to lymphocytes. Neoplastic transformation of these cells can occur at any of these lymphocyte maturation stages, giving rise to the different types of lymphoproliferative syndromes (LPS). This explains the great biological and clinical variety and heterogeneity of lymphomas. The lymphatic system is found in many parts of the body, so lymphomas can originate anywhere in the body.
The lymphatic system of the body, where lymphomas occur, consists of several organs or elements:
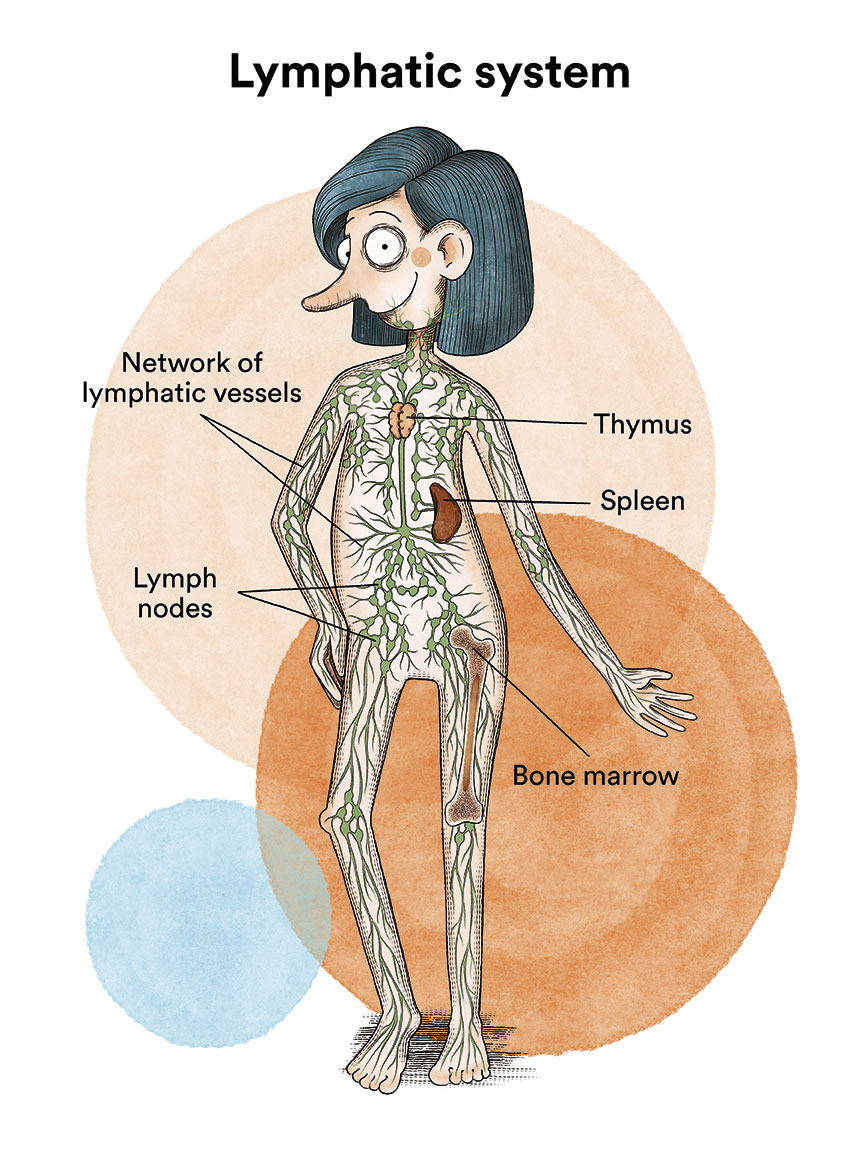
- Lymph: is a colourless, watery fluid that travels through the lymphatic vessels and carries T and B lymphocytes.
- Lymph vessels: is the network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.
- Lymph nodes: are small structures that can be found in different parts of the body such as the neck, armpits, abdomen, pelvis, groin or mediastinum (between the lungs). These lymph nodes filter lymph and help fight infection and disease.
- Spleen: is the organ that produces lymphocytes and stores red blood cells and lymphocytes. The spleen filters the blood and destroys old blood cells. The spleen is on the left side of the abdomen, near the stomach.
- Thymus: is the organ where lymphocytes mature and multiply. The thymus is in the chest behind the breastbone.
- Bone marrow: is the soft, spongy tissue located inside certain bones, such as the hip and sternum. It is commonly called “marrow”. Bone marrow produces the white blood cells, red blood cells and platelets. See Leukaemia, bone marrow and blood cells.
- Tonsils: are two small masses of lymph tissue at the back of the throat. There is one tonsil on each side of the throat.
What are the causes of Hodgkin’s lymphoma?
The causes of Hodgkin’s lymphoma are currently unknown. In principle, it is not an infectious or hereditary disease, there are no environmental factors that are clearly related to its development and, although the presence of the Epstein-Barr virus can be detected in some cases, the causal relationship between the virus and the development of the disease is not sufficiently understood at present, although numerous research groups are trying to elucidate this relationship.
According to the US National Cancer Institute, “it is possible that Epstein-Barr virus infection and a family history of Hodgkin’s lymphoma may increase the risk of childhood Hodgkin’s lymphoma”. This is called “risk factors” but in no way means that a person will develop cancer.
Risk factors for Hodgkin’s lymphoma include the following:
- Being infected with Epstein-Barr virus (EBV).
- Having a personal history of mononucleosis.
- Being infected with human immunodeficiency virus (HIV).
- Having certain immune system diseases, such as autoimmune lymphoproliferative syndrome.
- Having a weakened immune system after an organ transplant or from an immunosuppressive drug given to prevent the body from rejecting the organ.
- Having a parent, brother or sister with a personal history of Hodgkin’s lymphoma.
What are the symptoms of Hodgkin’s lymphoma?
In most cases, patients have no symptoms at the time of diagnosis (60-70% of them). The most frequent reason for consulting a doctor is the appearance of an enlarged lymph node. These lymph nodes are preferentially located in the cervical region (they are often mistaken for swollen lymph nodes secondary to oral, dental or ear infections). Sometimes these enlarged nodes are located in the axillary or inguinal region. Often, patients come to the doctor with a persistent dry cough and a chest X-ray shows a mass in the mediastinum (the region between the two lungs). More rarely, the patient has abdominal pain due to enlargement of the spleen. Only in 25-30% of cases does the patient present with so-called B symptoms (weight loss of more than 10% in the last six months without cause, evening fever and night sweats). Occasionally, patients may experience generalised skin itching and scratching lesions of several months’ duration before diagnosis of the disease (10-15% of patients) and lymph node pain appearing within minutes after alcohol intake (especially in young patients).
When there is fever, unexplained weight loss and excessive night sweats, this is known as B-symptoms. Their presence or absence at diagnosis is important in order to classify the lymphoma.
How is Hodgkin’s lymphoma diagnosed?
 The diagnosis of Hodgkin’s lymphoma must be made by biopsy of a suspicious lymph node. Needle aspiration of a swollen lymph node, a very frequently used strategy for the diagnosis of solid tumours in medical oncology, is not a valid technique for the diagnosis of lymphomas in general because it does not allow the structure of the lymph node to be seen under the microscope. In some cases, core needle biopsy can be used.
The diagnosis of Hodgkin’s lymphoma must be made by biopsy of a suspicious lymph node. Needle aspiration of a swollen lymph node, a very frequently used strategy for the diagnosis of solid tumours in medical oncology, is not a valid technique for the diagnosis of lymphomas in general because it does not allow the structure of the lymph node to be seen under the microscope. In some cases, core needle biopsy can be used.
From an anatomopathological point of view and according to the latest World Health Organization classification, Hodgkin’s lymphoma is divided into two main categories:
Classic Hodgkin’s lymphoma. Constituting 95% of all Hodgkin’s lymphomas, the characteristic cells are Reed Sternberg cells which characteristically express two membrane antigens, CD30 and CD15. The expression of CD30 is important when considering treatment of the disease with specific monoclonal antibodies. Classic Hodgkin’s lymphoma is subdivided into four different subtypes: nodular sclerosis subtype Hodgkin’s lymphoma (more frequent and more characteristic in young women), mixed cellularity subtype, lymphocyte-rich subtype and lymphocyte-depleted subtype (the rarest form and the one with the worst prognosis).
Nodular lymphocyte-predominant Hodgkin’s lymphoma. It is a very rare form, representing only 5% of cases, has a clinical course and evolution that is very different from classic Hodgkin’s lymphoma, the characteristic cells are the so-called pop corn cells which, characteristically, do not express CD30 or CD15, but do express CD20.
Once the diagnosis of the disease has been made, a study must be carried of the extent of the disease, i.e. it is necessary to know how much disease the patient has at the time of diagnosis, by means of the following tests:
- Blood tests (haemogram and biochemistry) with LDH, beta 2 microglobulin and complete serology
- Imaging test to detect the presence of pathological lymph nodes or other affected areas, with positron emission tomography associated with a computerised axial tomography (PET/CT) being the test of choice. In those cases where PET/CT is negative, a bone marrow biopsy is no longer recommended.
The extension study allows us to classify the patient into different stages according to the Ann Arbor staging:
- Stage I. The lymphoma affects a single lymph node region or affects a single organ outside the lymphatic system
- Stage II. Two or more lymph node regions are involved on the same side of the diaphragm
- Stage III. Multiple lymph node regions on both sides of the diaphragm are involved
- Stage IV. One or more extranodal territories (bone marrow, liver, lungs) are affected
The stage in the Ann Arbor staging is accompanied by the letters A, B, E or S:
- There are no B symptoms at diagnosis (fever, significant weight loss, night sweats)
- There are B symptoms
- There is involvement of an extranodal region by contiguity from the involvement of a lymph node or bundle of nodes
- There is involvement of the spleen
All these classifications make it possible to elucidate the risk group of the lymphoma diagnosed and thus to propose the most appropriate treatment.
What is the treatment for Hodgkin’s lymphoma?
Hodgkin’s lymphoma is the most common haematological cancer that we can cure at the moment. In recent years we have been able to significantly improve the long-term survival of patients, especially young patients. The treatment of Hodgkin’s lymphoma is based on the use of polychemotherapy sometimes associated with radiotherapy on the affected area, high-dose chemotherapy with autologous transplantation of haematopoietic progenitors and, at present, we also have the so-called “new drugs” for the treatment of this disease. The prognosis for patients who are primarily refractory to first-line treatment or who relapse after having achieved complete remission is no longer as favourable. It is important to re-biopsy clinically pathological nodes to demonstrate histological disease relapse.

“In June 2019 I was diagnosed with Hodgkin’s lymphoma and everything in my life began to change, work, projects, trips and a long etcetera were paused. Priorities also changed. Hospitals were at the top of the list, tests, chemo, and everything else took a backseat. When I was diagnosed, they told me all going to be a matter of 6 months of treatments, a little recovery from chemo, and I will be ready to go back into the world because Hodgkin’s lymphoma is one of the most curable blood cancers. But my plans went awry since they detected an early relapse. After an autologous bone marrow transplant, I relapsed again and, finally, in 2021, I underwent a transplant from an unrelated donor located by the Foundation’s REDMO program. Wherever you are, THANK YOU to my donor and to all those who are registered in REDMO, I hug you with my soul, but, above all, full of LIFE thanks to my donor.” 
Lucas, 38 years old.
Hodgkin’s lymphoma.
First-line treatment.
In our setting, the chemotherapy regimen considered standard is ABVD (combination of adriamycin, bleomycin, vinblastine and dacarbazine). ABVD is administered intravenously on an outpatient basis in most patients, the cycle is repeated every 28 days with two administrations, one on day 1 and the second on day 14. For patients diagnosed in early stages without poor prognostic factors, the recommended treatment is the administration of two cycles of ABVD and complementary radiotherapy on affected fields (20 Gys). In patients diagnosed in early stages, but with poor prognostic factors, four cycles of ABVD and adjuvant radiotherapy (30 Gys) are recommended. Treatment of advanced stage patients involves six cycles of ABVD. If the PET/CT scan at the end of chemotherapy is negative, adjuvant radiotherapy is generally not necessary.
There are other more intensive chemotherapy regimens, more effective in controlling the disease, but also more toxic, which are not very frequently used in our country (e.g. escalated BEACOPP).
Second-line and subsequent treatment.
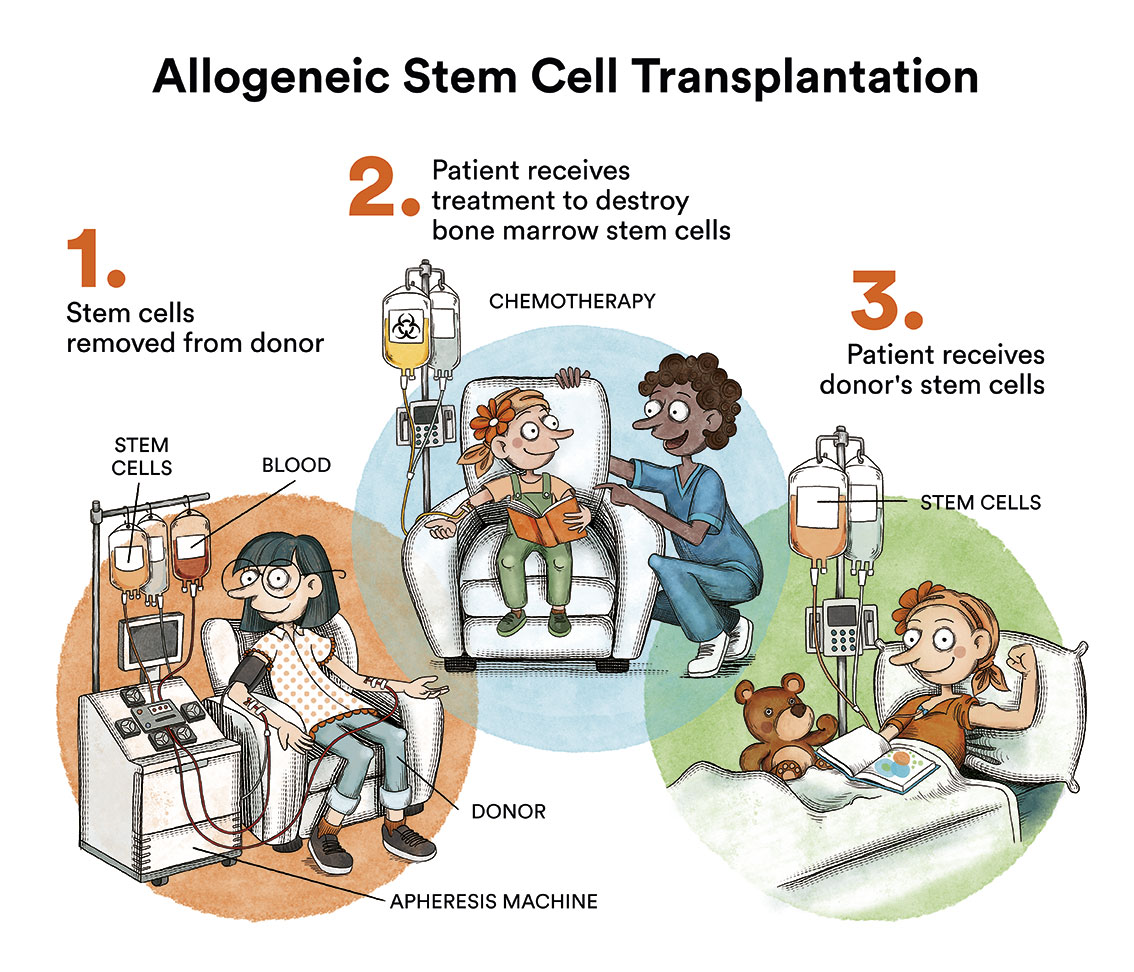
Although the results of first-line treatment are very good, there are 5-15% of patients who are primarily refractory (non-responders to first-line treatment) and 30% of patients who, after achieving complete remission, subsequently relapse. These patients are treated with second-line chemotherapy regimens. These treatments are more intensive than first-line treatments and, above all, use different drugs than those included in the first-line treatment. If the patient achieves a response, consolidation with high-dose chemotherapy and autologous haematopoietic stem cell transplantation is indicated.
Patients who relapse after autologous transplantation have a worse prognosis. Until relatively recently, patients who relapsed after autologous transplantation could be candidates for allogeneic haematopoietic stem cell transplantation from an identical sibling, a matched unrelated donor and, more recently, from a haploidentical family donor.
We now have “new drugs” in the treatment of Hodgkin’s lymphoma that are currently indicated for patients who are relapsed or refractory to previous treatment. The first of these is brentuximab vedotin, a monoclonal antibody anti-CD30 that has been shown to be very effective with a very acceptable toxicity profile in relapsed or refractory patients after autologous transplantation or in patients who have failed two different lines of prior chemotherapy and are not candidates for autologous haematopoietic stem cell transplantation.
The second group of new drugs we are currently using in the treatment of these patients are the so-called checkpoint inhibitors (nivolumab, pembrolizumab) which are currently indicated in patients who relapse after autologous transplantation and who also fail treatment with brentuximab vedotin. Nivolumab and pembrolizumab are also very effective and well tolerated by most patients.
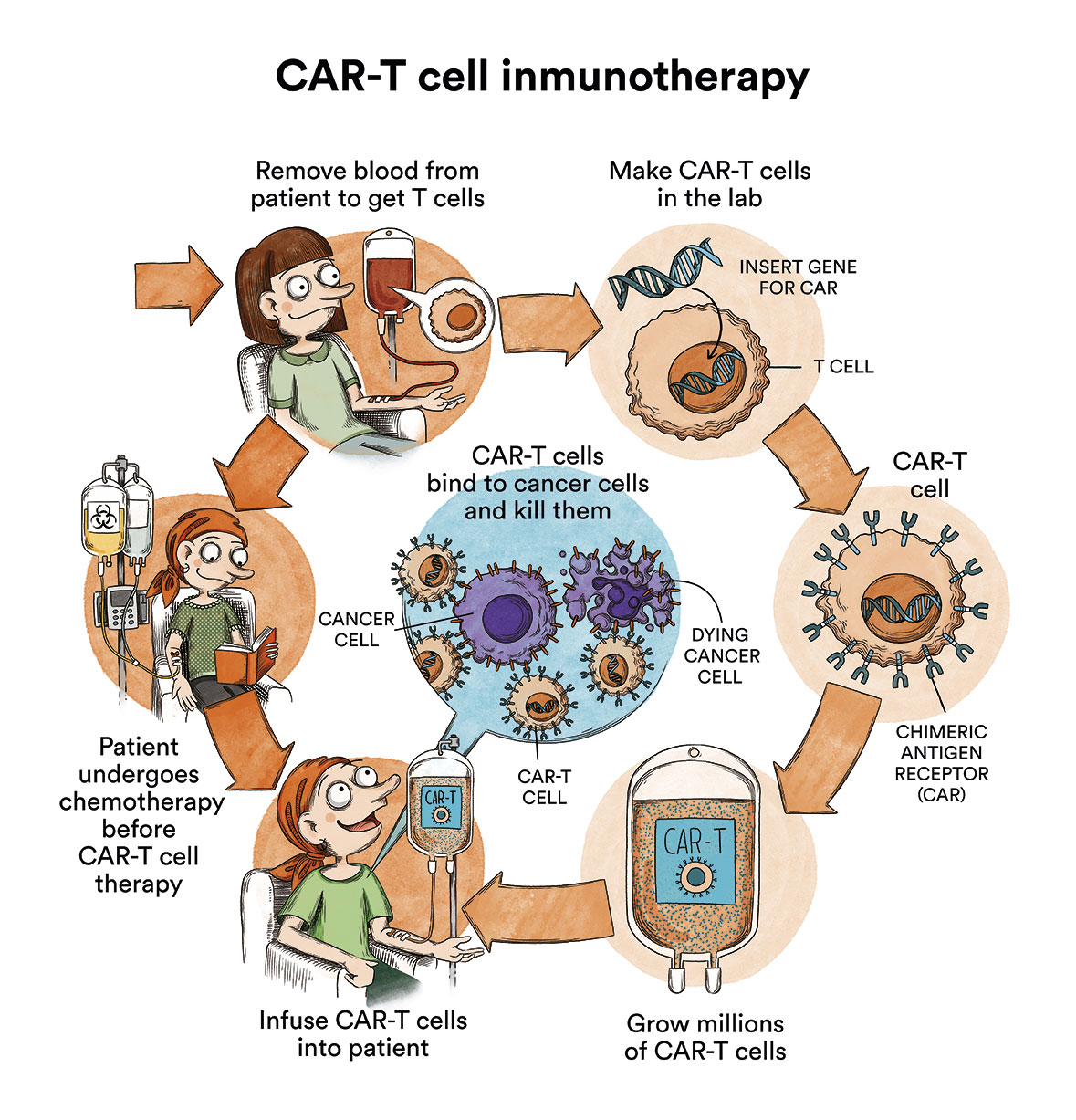
Other treatments are being tested in clinical trials. A treatment clinical trial is a research study to improve current treatments or obtain information on new treatments for cancer patients. A number of clinical trials of CAR-T immunotherapies (content in spanish) anti CD-30 (a protein expressed by the cancer cells of many types of Hodgkin’s lymphoma) are currently underway around the world for patients who have exhausted all therapeutic options in the pipeline.

Claudia
Hodgkin lymphoma.
“Me convertí en Imparable, sin quererlo, en mayo de 2014. Desde entonces “I became Unstoppable, unintentionally, in May 2014. Since then, I have lived many adventures, but, without a doubt, my favourite one is being part of the Josep Carreras Foundation team. It all started with the diagnosis. I was living in Hamburg and on a visit in Spain, I decided to go to the doctor. What a scare. I had to move back to my parents’ house, leave my job, my friends… My whole life was put on hold. It was a Hodgkin’s lymphoma. Doctors started treating myself with chemotherapy, but soon everything got complicated. I had several relapses, underwent an autotransplant and then a bone marrow transplant. My brother Edu was my donor and thanks to him I have LIVED again. I know that I have told you my story in a very short way, but if you want you can read my ebook (in Spanish).”
What are the chances of adult Hodgkin’s lymphoma patients being cured?
As with any neoplastic disease, prognosis depends on the histological type of Hodgkin’s lymphoma, its extent and response to treatment. If there are no adverse factors, and they have been correctly treated, the probability of cure for these patients is over 80%.
Despite the generally good prognosis of patients with Hodgkin’s lymphoma, patients who do not achieve complete remission after initial treatment or patients with late relapses have a much poorer prognosis.
Links of interest concerning medical issues relating to Hodgkin’s lymphoma
Hodgkin Lymphoma. American Cancer Society
Hodgkin lymphoma. Cancer Research UK
Hodgkin Lymphoma (HL). Leukemia & Lymphoma Society
Adult Hodgkin Lymphoma Treatment. National Cancer Institute
Hodgkin lymphoma. Blood Cancer UK
Links of interest on other topics related to Hodgkin’s lymphoma:
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia or cancer patients:
In Spain there is a large network of associations for haematological cancer patients that, in many cases, can inform you, advise you and even carry out certain procedures. These are the contacts of some of them by Autonomous Communities:
All these organisations are external to the Josep Carreras Foundation.
STATE
- AMILO (Asociación Española de Amiloidosis)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- JOSEP CARRERAS LEUKAEMIA FOUNDATION
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


