Non-Hodgkin’s lymphomas
Lymphomas (or cancers of the lymphatic system) are classified into two main types: Hodgkin’s lymphoma and non-Hodgkin’s lymphomas. The latter, in turn, can be indolent (chronic) or aggressive. There are more than 60 different subtypes of non-Hodgkin’s lymphoma with completely different prognoses and treatments.
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.

Information reviewed by Dr. Rocío Parody Porras, Doctor specialising in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
What is lymphoma?
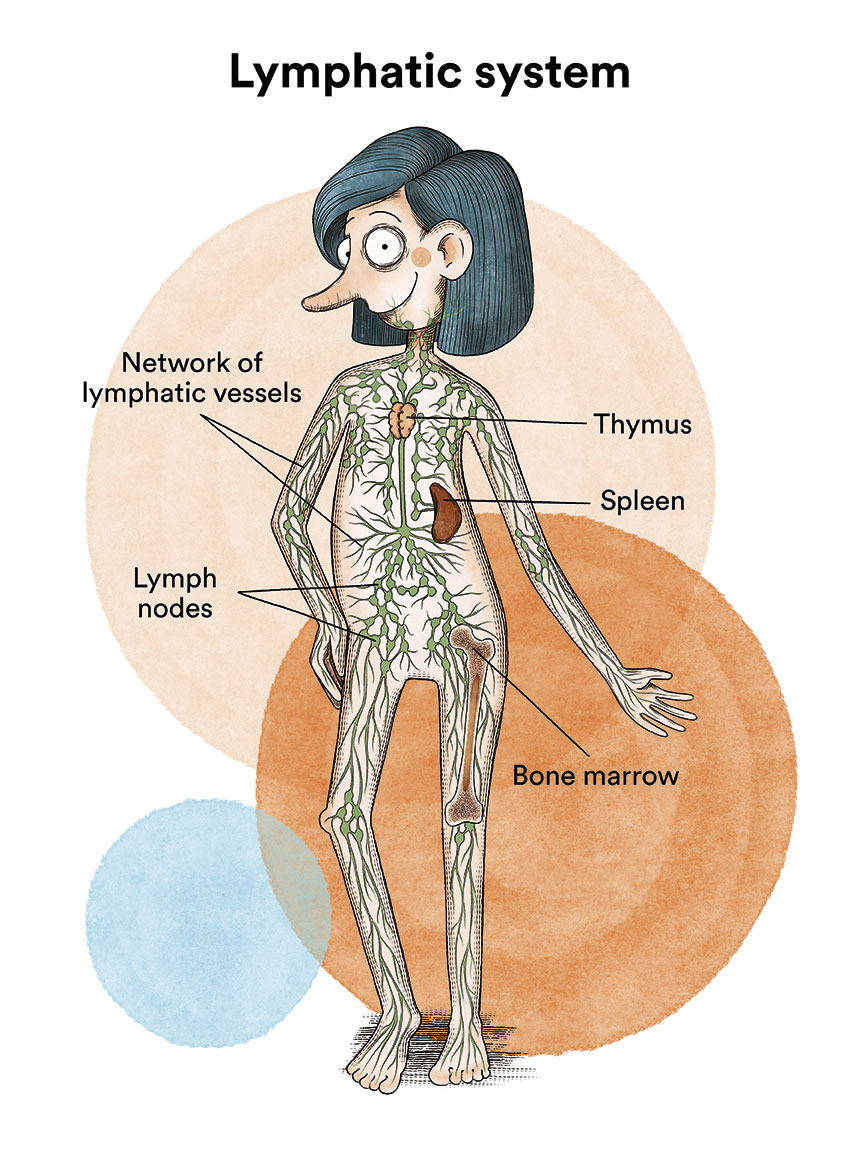
A lymphoma is a type of cancer of the blood, specifically of the lymphatic system. The lymphatic system is a network of organs (spleen and thymus), lymph nodes, lymph ducts and vessels that produce and transport lymph from the tissues to the bloodstream. It is a key part of our body’s immune system and helps protect the body against germs, including bacteria and viruses.
The lymphatic system is primarily made up by cells known as lymphocytes, which are a type of white blood cells. There are two main types of lymphocytes in our blood, called B-lymphocytes (B cells) and T-lymphocytes (T cells).
- B-lymphocytes: They make up 5-15% of all lymphocytes and give rise to plasma cells that produce antibodies and help protect the body against bacteria or viruses. Antibodies attach to germs, and mark them for destruction by other components of the immune system.
- T-lymphocytes: They are responsible for coordinating the cellular immune response and are responsible for cooperation in the development of all forms of immune response, including the production of antibodies by B-lymphocytes. There are several types of T-cells, each with a special function. Some T-cells destroy germs or abnormal cells in the body. Other T-cells stimulate or slow down the activity of other immune system cells.
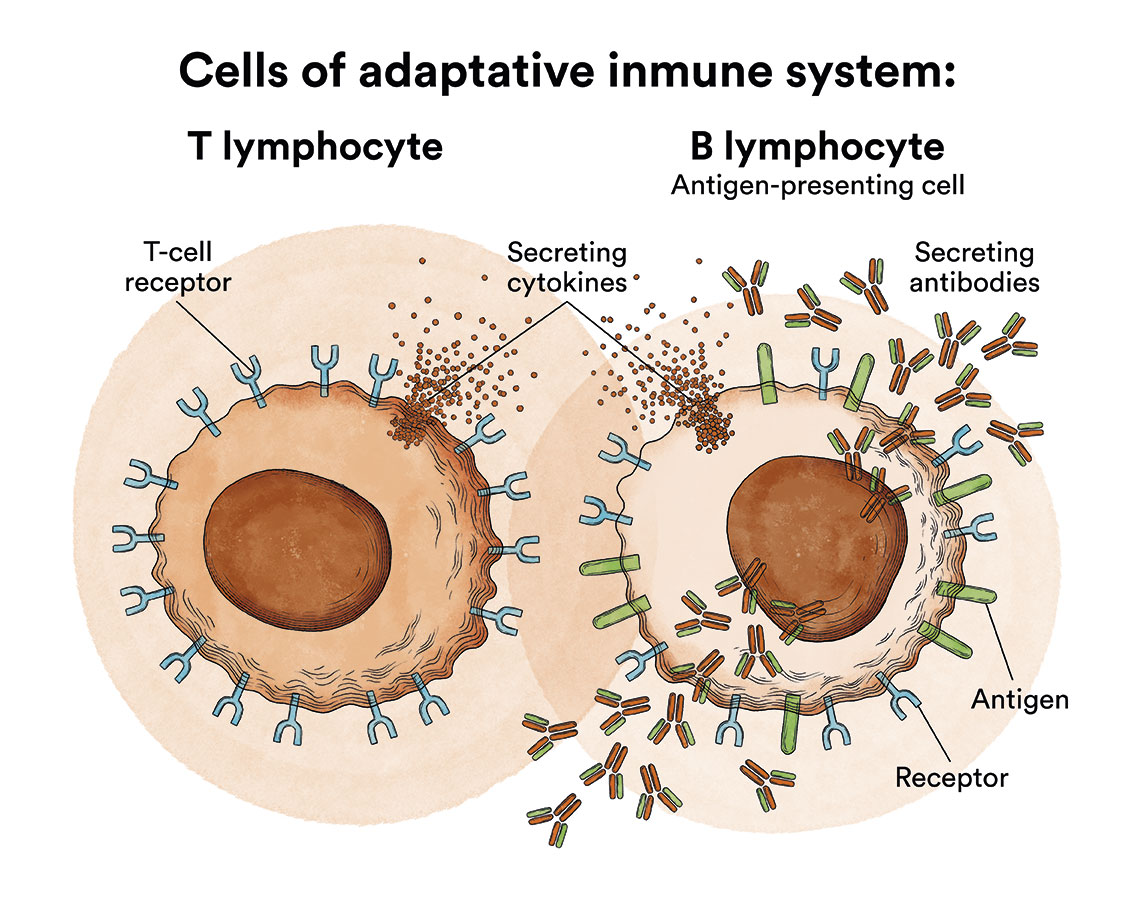
Circulating B and T lymphocytes are derived, like all blood cells, from haematopoietic stem cells in the bone marrow. The stem cell gives rise, among others, to lymphoblasts (more immature lymphoid cells) and from these, after successive maturation stages, to lymphocytes. Neoplastic transformation of these cells can occur at any of these lymphocyte maturation stages, giving rise to the different types of lymphoproliferative syndromes (LPS). This explains the great biological and clinical variety and heterogeneity of lymphomas. The lymphatic system is found in many parts of the body, so lymphomas can originate anywhere in the body.
The lymphatic system of the body, where lymphomas occur, consists of several organs or elements:
- Lymph: is a colourless, watery fluid that travels through the lymphatic vessels and carries T and B lymphocytes.
- Lymph vessels: is the network of thin tubes that collect lymph from different parts of the body and return it to the bloodstream.
- Lymph nodes: are small structures that can be found in different parts of the body such as the neck, armpits, abdomen, pelvis, groin or mediastinum (between the lungs). These lymph nodes filter lymph and help fight infection and disease.
- Spleen: is the organ that produces lymphocytes and stores red blood cells and lymphocytes. The spleen filters the blood and destroys old blood cells. The spleen is on the left side of the abdomen, near the stomach.
- Thymus: is the organ where lymphocytes mature and multiply. The thymus is in the chest behind the breastbone.
- Bone marrow: is the soft, spongy tissue located inside certain bones, such as the hip and sternum. It is commonly called “marrow”. Bone marrow produces the white blood cells, red blood cells and platelets. See Leukaemia, bone marrow and blood cells.
- Tonsils: are two small masses of lymph tissue at the back of the throat. There is one tonsil on each side of the throat.
Types of lymphomas

Yaiza
Non-Hodgkin’s lymphoma.
“When I turned 21 I was diagnosed with lymphoma. I had a 14cm tumor in the mediastinum that collapsed a lung and displaced my heart. We had to start chemotherapy as soon as possible. I am a very optimistic person, so when they told me that because of my youth I had a good chance of overcoming it in a few months, I stuck to it and faced the treatment with great enthusiasm.
Despite this, the results were not good, and I had to undergo an autologous bone marrow transplant, an experimental treatment and, subsequently, a transplant from my brother. That’s how, after 5 years, I achieved the complete remission. There have been many years of relentless suffering, anguish, and fear, but I am grateful and happy to be able to explain all this in the past tense. Now, with my experience, I help patients and families with first-hand information through social networks (in Spanish) so that cancer and everything that it entails stops being a taboo topic and those newly diagnosed can better understand each part of their disease.”
Lymphomas are usually classified into two main types:
- Hodgkin’s lymphoma
Currently, according to the latest data from the Spanish Society of Medical Oncology (SEOM), more than 1,500 cases of Hodgkin’s lymphoma are diagnosed each year in Spain.
- Non-Hodgkin’s lymphomas
Likewise, within this large heterogeneous group there can be aggressive lymphomas and indolent (“chronic”) lymphomas, depending on the speed of growth and the specific characteristics of the tumour cell. Lymphomas are further classified depending on whether the affected cell is a B-cell or a T-cell. Currently, according to the latest data from the Spanish Society of Medical Oncology (SEOM), more than 9,000 cases of non-Hodgkin’s lymphoma are diagnosed each year in Spain.
Hodgkin’s lymphoma is usually a single clinical entity with several stages, while there are more than 60 types of non-Hodgkin’s lymphoma (NHL) with radically different treatments and prognoses.
From a practical point of view, non-Hodgkin’s lymphomas can be divided into two main groups based on their growth rate.
- Aggressive lymphomas, also known as high-grade lymphomas, tend to grow and spread rapidly and often cause severe symptoms. The most common are diffuse large B-cell lymphoma (1/3 of all lymphomas), mantle cell lymphoma, peripheral T-lymphoma, Burkitt’s lymphoma and lymphoblastic lymphoma (equivalent to a type of acute lymphoblastic leukaemia).
- Indolent lymphomas, also called low-grade lymphomas, have a less aggressive behaviour, with lymphadenopathies of years of evolution and a preserved general condition, although they are usually very widespread (stages III and IV). The most common are follicular lymphoma, small lymphocyte lymphoma (equivalent to chronic lymphocytic leukaemia), lymphoplasmacytic lymphoma/Waldenström macroglobulinemia), marginal zone lymphoma (including MALT lymphomas) and cutaneous T-lymphomas (mycosis fungoides and Sézary syndrome).
Paradoxically, aggressive non-Hodgkin’s lymphomas usually respond well to chemotherapy treatments, whereas indolent lymphomas are very difficult to eradicate completely, although with current treatments patients can live for many years and most of the time without symptoms.
In this section we will develop or redirect to quality information for patients with some of the types of non-Hodgkin’s lymphoma (NHL):
- Follicular lymphoma
- Diffuse large B-cell lymphoma
- Mantle cell lymphoma
- Lymphoblastic lymphoma
- Burkitt’s lymphoma
- MALT-type extranodal B-cell lymphoma
- Anaplastic large cell lymphoma
- Peripheral T lymphomas
- Cutaneous T lymphomas: Mycosis fungoides and Sézary syndrome
The causes of non-Hodgkin’s lymphomas (NHL), the clinical features, the diagnostic work-up and the staging of the disease are common to all lymphomas, as discussed below. The specific features of some of them (whether at diagnosis they are more frequently localised or disseminated, or the site of onset) will be detailed in each corresponding section
What are the causes of non-Hodgkin’s lymphoma?
The causes for the development of NHL are currently unknown, except in specific cases such as Burkitt’s lymphoma, which may be associated with reactivation of the Epstein Barr virus, or immunodeficiencies secondary to HIV or previous immunosuppressive treatment. It is therefore not generally an infectious or hereditary disease, nor are there environmental factors that are clearly related to its development.
What are the symptoms of non-Hodgkin’s lymphoma?
The most frequent cause for consulting a doctor, as in other types of lymphoma, is the appearance of a painless and enlarged lymph node. These lymph nodes are preferably located in the cervical region (they are often mistaken for swollen lymph nodes secondary to oral, dental or ear infections). Sometimes these enlarged nodes are located in the axillary or inguinal region. Often, patients come to the doctor with a persistent dry cough and a chest X-ray shows a mass in the mediastinum (the region between the two lungs).
In some cases, the patient presents with the so-called B symptoms (weight loss of more than 10% in the last six months without cause, evening fever and night sweats), as well as fatigue.
In indolent NHL, it is not uncommon for the diagnosis to be made in asymptomatic individuals in whom imaging or laboratory tests are performed for other reasons.
How is non-Hodgkin’s lymphoma diagnosed?
 The diagnosis of NHL should be reached by means of the following tests, which will also allow staging of the disease (if it is localised in one or several areas, or even disseminated by affecting the bone marrow and therefore the blood):
The diagnosis of NHL should be reached by means of the following tests, which will also allow staging of the disease (if it is localised in one or several areas, or even disseminated by affecting the bone marrow and therefore the blood):
- Physical examination and medical history.
- Blood tests (haemogram and biochemistry including tumour markers such as LDH and Beta2 microglobulin in blood, as well as serology of infectious markers). Lymphocyte immunophenotyping studies can be performed in this analysis if there is suspicion of lymphoma infiltration in the blood.
- Imaging test to detect the presence of pathological lymph nodes or other affected areas (at present, the test to be used is positron emission tomography associated with a computerised axial tomography – PET/CT) and, in those cases in which PET/CT is negative, it is no longer recommended to perform a bone marrow biopsy.
- Biopsy of a suspicious lymph node is the test of choice, whereas puncture/aspiration of a swollen lymph node is not a valid technique as it does not allow the structure of the node to be seen under the microscope. Core needle biopsy can be used in some cases. The histological study (of the lymph node tissue) should always be completed with an immunohistochemical, cytogenetic study (to rule out chromosomal alterations that are typical of some types of lymphoma) and molecular study to make a correct differential diagnosis with other very similar lymphomas.
- Electrocardiogram and chest X-ray, which allows for evidence of mediastinal widening (centrothoracic mass that may be the origin of a lymphoma)
- PET/CT with thoracic, abdominal and pelvic CT.
- Bone marrow biopsy (not necessary if PET/CT is negative).
- Lumbar puncture (flow cytometry +/- cytology): indicated in patients at high risk of CNS involvement such as those with testicular, breast, renal, epidural or epidural involvement or when there is more than one extranodal location and very high LDH (as typically occurs in lymphoblastic lymphoma, Burkitt’s lymphoma and diffuse large cell lymphoma).
The following tests can be used to determine the extent of the disease:
- Stage I: Involvement of a single nodal territory or a single site.
- Stage II: Involvement of two or more nodal territories or lymphoid structures on the same side of the diaphragm.
- Stage III: Involvement of lymph node territories or lymphoid structures on both sides of the diaphragm.
- Stage IV: Lymphoma spread to other organs (e.g. bone marrow, liver, etc.)
In addition, depending on the presence of general B symptoms (weight loss ≥10% during the previous six months unexplained by other reasons, fever >38°C persistent or remitting for one month prior to diagnosis, profuse night sweats during the previous month), each of these stages is subclassified into A, B, E or S:
- A: The patient has none of the above-mentioned B symptoms.
- B: The patient has one or more of the B symptoms.
- E: Lymphoma is located in an organ or tissue other than a lymph node or the spleen.
- S: When the spleen is affected by lymphoma
Links of interest on other topics related to non-Hodgkin’s lymphoma:
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia, lymphoma or cancer patients:
In Spain there is a large network of associations for haematological cancer patients which, in many cases, can provide information, advice and even carry out certain procedures. These are the contacts of some of them by Autonomous Community:
All these organisations are external to the Josep Carreras Foundation.
STATE
- AMILO (Asociación Española de Amiloidosis)
- ACLIF (Asociación para la cura del linfoma folicular)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- JOSEP CARRERAS LEUKAEMIA FOUNDATION
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
COMUNIDAD VALENCIANA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


